Tug'ilish - Childbirth
| Tug'ilish | |
|---|---|
| Boshqa ismlar | Mehnat va tug'ish, tug'ish va tug'ish, partus, tug'ish, tug'ish, tug'ilish, qamoq[1][2] |
 | |
| Yangi tug'ilgan chaqaloq va ona | |
| Mutaxassisligi | Akusherlik, doya |
| Asoratlar | To'siq qilingan mehnat, tug'ruqdan keyingi qon ketish, eklampsi, tug'ruqdan keyingi infektsiya, tug'ilish asfiksiyasi, neonatal gipotermiya[3][4][5] |
| Turlari | Vaginal etkazib berish, C bo'limi[6][7] |
| Sabablari | Homiladorlik |
| Oldini olish | Tug'ilishni nazorat qilish, abort |
| Chastotani | 135 million (2015)[8] |
| O'limlar | 500,000 onalar o'limi yil[5] |
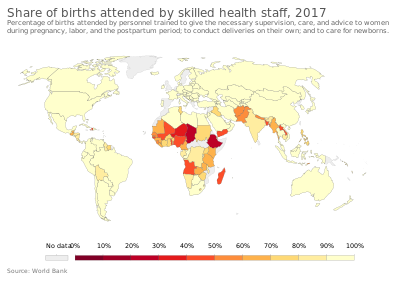
Tug'ilish, shuningdek, nomi bilan tanilgan mehnat va etkazib berish, oxiri homiladorlik qaerda bir yoki bir nechta Chaqaloqlar qoldiradi bachadon orqali o'tib qin yoki tomonidan Kesariya bo'limi.[7] 2015 yilda ularning soni 135 millionga yaqin edi tug'ilish global miqyosda.[8] Taxminan 15 million tug'ilgan homiladorlikning 37 xaftaligidan oldin,[9] 3 dan 12 foizgacha tug'ilganlar 42 haftadan so'ng.[10] In rivojlangan dunyo ko'pincha etkazib berish kasalxonalarda,[11][12] ichida rivojlanayotgan dunyo aksariyat tug'ilishlar a ko'magi bilan uyda ro'y beradi an'anaviy tug'ilish xizmati.[13]
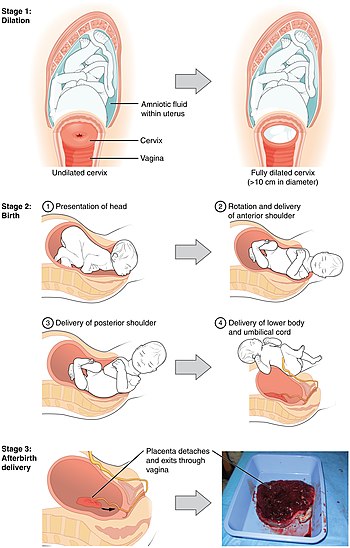
Tug'ilishning eng keng tarqalgan usuli bu qin orqali etkazib berish.[6] U mehnatning uch bosqichini o'z ichiga oladi: qisqartirish va bachadon bo'yni ochilishi birinchi bosqichda, ikkinchi bosqichda chaqaloqning tushishi va tug'ilishi va tug'ilishi platsenta uchinchi bosqich davomida.[14][15] Birinchi bosqich qorin yarim yoki bel og'rig'i bilan boshlanadi va yarim daqiqada davom etadi va har 10-30 daqiqada yuz beradi.[14] Vaqt o'tishi bilan og'riq kuchayib, bir-biriga yaqinlashadi.[15] Ikkinchi bosqich chaqaloq to'liq chiqarib yuborilganda tugaydi. Uchinchi bosqichda platsentani etkazib berish, kindik ichakchasini kechiktirish odatda tavsiya etiladi.[16] 2014 yildan boshlab,[yangilash] barcha yirik sog'liqni saqlash tashkilotlari qinidan tug'ilgandan so'ng yoki sezaryen so'ng onasi sergak va sezgir bo'lishi bilanoq, chaqaloqni onaning ko'kragiga yotqizish, deb atashadi teridan teriga aloqa, muntazam protseduralarni kamida bir-ikki soatga kechiktirish yoki chaqaloq birinchi marta emizguncha.[17][18][19]
Ko'pincha chaqaloqlar tug'iladi birinchi bosh; ammo taxminan 4% birinchi bo'lib tug'ilgan oyoq yoki dumba, deb nomlanadi kam.[15][20] Odatda bosh tos suyagiga bir tomonga qarab kiradi va keyin pastga qarab aylanadi.[21] Tug'ruq paytida, ayol odatda ovqat eyishi va xohlagan joyida harakatlanishi mumkin.[22] Kabi bir qator usullar og'riq bilan yordam beradi yengillik texnikasi, opioidlar va orqa miya bloklari.[15] An deb nomlanuvchi qinning ochilishiga kesim yasash paytida epizyotomiya, tez-tez uchraydi, odatda kerak emas.[15] 2012 yilda sezaryen bilan 23 millionga yaqin tug'ruq amalga oshirildi, bu qorin bo'shlig'i operatsiyasi.[23][15]
Har yili homiladorlik va tug'ruq paytida tug'ruq asoratlari 500 mingga yaqinni tashkil qiladi onalar o'limi, etti million ayol jiddiy uzoq muddatli muammolarga duch kelmoqda va tug'ruqdan keyin 50 million ayol sog'lig'ining salbiy natijalariga ega.[5] Ularning aksariyati rivojlanayotgan dunyo.[5] Maxsus asoratlar kiradi to'siq qilingan mehnat, tug'ruqdan keyingi qon ketish, eklampsi va tug'ruqdan keyingi infektsiya.[5] Boladagi asoratlar o'z ichiga olishi mumkin tug'ilish paytida kislorod etishmasligi, tug'ilish travması, erta tug'ilish va infektsiyalar.[4][24]
Belgilari va alomatlari

(Izoh: Ushbu maqola ba'zi atamalar uchun ingliz imlosidan foydalanadi. AQShda "mehnat" emas, "mehnat" imlosi odatda ishlatiladi.) Mehnatning eng ko'zga ko'ringan belgisi kuchli takrorlanuvchi bachadonning qisqarishi. Mehnatkash ayollar tomonidan bildirilgan qayg'u darajasi har xil. Ularga qo'rquv va xavotirlik darajasi, tug'ilishdan oldingi tajriba, tug'ruq paytida og'riqning madaniy g'oyalari, mehnat paytida harakatchanlik va mehnat paytida olingan yordam ta'sir ko'rsatmoqda.[25][26] Shaxsiy kutishlar, parvarish qiluvchilarning yordami miqdori, parvarish qiluvchi bilan bemorning munosabatlar sifati va qaror qabul qilishda ishtirok etish ayollarning yoshi, ijtimoiy-iqtisodiy holati, millati, tayyorgarligi kabi boshqa omillarga qaraganda tug'ilish tajribasidan qoniqishida muhimroqdir. , jismoniy muhit, og'riq, harakatsizlik yoki tibbiy aralashuvlar.[27]
Ta'riflar
Kasılmalardaki og'riq, juda kuchli hayz kramplarına o'xshash tuyg'u sifatida tasvirlangan. Ayollarni ko'pincha qichqiriqdan tiyilishga chaqirishadi. Biroq, og'riqni kamaytirishga yordam beradigan nola va xo'rsinga da'vat qilish mumkin. Qarama-qarshilik kuchli cho'zish va yonish kabi tajribaga ega bo'lishi mumkin. Tug'ruq og'rig'iga ozgina ta'sir ko'rsatadigan ayollar ham, boshqa ayollarga qaraganda, toj kiyishga (chaqaloq boshining ko'rinishi) sezilarli darajada qattiq ta'sir ko'rsatadi.
Orqa mehnat bu pastki orqa qismida paydo bo'ladigan aniq og'riq uchun atama dum suyagi, tug'ruq paytida.[28]
Psixologik
Homiladorlikning keyingi bosqichlarida ko'pligi ko'paymoqda oksitotsin, mamnunlik hissi, xavotirning pasayishi va turmush o'rtog'i atrofida xotirjamlik va xavfsizlik hissi tug'diradigan gormon.[29] Tug'ruq paytida oksitotsin homila bachadon bo'yni va qinni qo'zg'atganda ham ajralib chiqadi va bu onaning go'dak bilan bog'lanishida va onalik xulq-atvorini o'rnatishda katta rol o'ynaydi deb ishoniladi. Bolani emizish harakati ham oksitotsinning ajralishini keltirib chiqaradi.[30]
Qo'shma Shtatlardagi onalarning 70% dan 80% gacha bo'lganida, tug'ilgandan keyin ba'zi qayg'u yoki "chaqaloq ko'k" hissi paydo bo'ladi. Odatda alomatlar har kuni bir necha daqiqadan bir necha soatgacha sodir bo'ladi va ular tug'ilgandan keyin ikki hafta ichida kamayishi va yo'qolishi kerak. Tug'ilgandan keyingi depressiya ba'zi ayollarda rivojlanishi mumkin. Profilaktik guruh terapiyasi tug'ruqdan keyingi depressiyani profilaktik davolash sifatida samarali ekanligini isbotladi.[31][32]
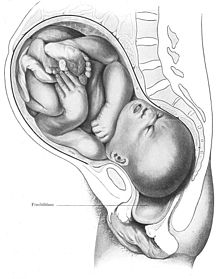
Vaginal tug'ilish
Odamlar tik turish bilan ikki oyoqli. Tik turgan holat qorin bo'shlig'i tarkibidagi narsalarning og'irligini ko'tarilishiga olib keladi tos suyagi, bu og'irlikni nafaqat qo'llab-quvvatlabgina qolmay, balki ayollarda uchta kanal o'tishiga imkon beradigan murakkab tuzilma siydik yo'li, qin va to'g'ri ichak. Kichkintoyning boshi va elkalari onaning tos suyagi halqasidan o'tishi uchun ma'lum bir manevrlar ketma-ketligidan o'tishi kerak.
Odatda vertexning oltita bosqichi yoki sefalik (bosh-birinchi taqdimot) etkazib berish:
- Nishon ning homila boshi ko'ndalang holatidadir. Bolaning boshi onaning bir yoki boshqa sonida tos suyagi bo'ylab joylashgan.
- Tushish va egilish homila boshi.
- Ichki aylanish. Xomilaning boshi 90 darajagacha buriladi oksipito-oldingi holat shunday qilib bolaning yuzi onaning to'g'ri ichak tomoniga qarab turadi.
- Kengaytma orqali etkazib berish. Xomilaning boshi egilib, ko'kragiga iyak qo'yiladi, shunda uning orqa yoki toji tug'ilish kanali orqali o'tishi kerak, bunda uning orqa qismi qovoq suyagiga bosilib, iyagi ko'kragidan chiqib, bo'ynini cho'zadi. agar yuqoriga qarash kerak bo'lsa va uning qolgan qismi tug'ilish kanalidan chiqib ketsa.
- Qayta tiklash. Xomilaning boshi hali ham burchak ostida bo'lgan elkalari bilan normal munosabatlarini tiklash uchun 45 darajadan buriladi.
- Tashqi aylanish. Elkalar boshning tirnoqli harakatlarini takrorlaydi, bu esa homila boshining so'nggi harakatlarida ko'rinadi.
Chaqaloq bu qismga kirganda qin "tug'ilish kanali" deb nomlanadi.
Stantsiya xomilaning joylashadigan qismining iskial o'murtqa darajasiga bog'liqligini anglatadi. Taqdim etilgan qism iskial tizmalarda bo'lganda, stantsiya 0 ga teng (qo'shilish bilan sinonim). Agar homilaning taqdim etilayotgan qismi tikanlardan yuqori bo'lsa, masofa o'lchanadi va minus stantsiyalar sifatida tavsiflanadi, ular -1 dan -4 sm gacha. Agar taqdimot qismi iskial tikanlar ostida bo'lsa, masofa plyus stantsiyalari (+1 dan +4 sm gacha) deb belgilanadi. +3 va +4 da taqdimot qismi perineumda joylashgan va uni ko'rish mumkin.[33]
Xomilaning boshi tug'ilish kanali bo'ylab harakatlanayotganda vaqtincha shaklini sezilarli darajada o'zgartirishi (cho'zilib ketishi) mumkin. Xomilalik bosh shaklidagi bu o'zgarish deyiladi qoliplash va birinchi marta qin bilan etkazib beriladigan ayollarda ancha mashhur.[34]
Servikal pishib etish bachadon bo'yni va tug'ilish kanaliga o'tishda sodir bo'ladigan cho'zilishga tayyorlash uchun bachadon bo'yni fizikaviy va kimyoviy o'zgarishlardir. A deb nomlangan ballar tizimi Bishop ballari bachadon bo'yni pishishi darajasini baholash uchun, tug'ruq va tug'ruq vaqtini taxmin qilish yoki muddatidan oldin tug'ilish xavfi ostida bo'lgan ayollar uchun foydalanish mumkin. Bundan tashqari, ayol qachon javob berishini baholash uchun ishlatiladi mehnatni induktsiya qilish tug'ruqdan keyingi homiladorlik yoki boshqa tibbiy sabablarga ko'ra. Bachadonning qisqarishini serviksni samarali ravishda kengaytirishga imkon beradigan bachadon bo'yni pishishini induktsiya qilishning bir necha usullari mavjud.[35]
Mehnat boshlanishi

Tug'ilish boshlanishining turli xil ta'riflari mavjud, jumladan:
- Bachadonning muntazam ravishda qisqarishi kamida har olti daqiqada o'zgarishi haqida dalolat beradi bachadon bo'yni kengayishi yoki bachadon bo'yni oqishi ketma-ket raqamli tekshiruvlar o'rtasida.[36]
- 10 daqiqadan kam vaqt oralig'ida yuzaga keladigan muntazam kasılmalar va bachadon bo'yni kengayishi yoki serviks chiqishi.[37]
- 10 daqiqalik davrda kamida uchta og'riqli muntazam bachadon qisqarishi, ularning har biri 45 sekunddan ko'proq davom etadi.[38]
Ko'proq bir xil terminologiyadan foydalanish uchun mehnatning birinchi bosqichi "yashirin" va "faol" bosqichlarga bo'linadi, bu erda yashirin faza ba'zan mehnatning ta'rifiga kiradi,[39] va ba'zida yo'q.[40]
Odatda mehnat deb ataladigan mehnatning boshlanishiga yaqin bo'lgan umumiy belgilarga "yorug'lik" kiradi. Yoritish - bu bolaning boshi tos suyagiga chuqur kirib, qovurg'a qafasidan pastga tushadigan jarayon. Keyin homilador ayol nafas olishni osonlashtirishi mumkin, chunki uning o'pkasida kengayish uchun ko'proq joy bor, ammo siydik pufagiga bosim tez-tez bo'shatilishi kerak (siydik chiqarish). Yorug'lik tug'ilish boshlanishidan bir necha hafta yoki bir necha soat oldin, hatto tug'ilish boshlangunga qadar sodir bo'lishi mumkin.[41]
Ba'zi ayollar, shuningdek, tug'ruq boshlanishidan bir necha kun oldin "shilimshiq tiqin", qalin tiqin paydo bo'lganda, qindan ajralishni ko'paytiradi mukus bachadonning ochilishini to'sib qo'yadigan va qinga chiqarib yuborilgan. Balg'am tiqilishi tug'ruq boshlanishidan bir necha kun oldin yoki tug'ilish boshlangunga qadar bo'lmasligi mumkin.[41]
Bachadon ichida bola suyuqlik bilan to'ldirilgan membrana bilan o'ralgan amniotik qop. Bir oz oldin, tug'ilish paytida yoki boshida xaltachaning yorilishi. "Suv uziladi" deb nomlangan xaltachaning yorilishi natijasida chaqaloq yuqtirish xavfi ostida bo'ladi va onaning tibbiy guruhi bunga ehtiyojni baholaydi mehnatni kuchaytirish agar u boshlanmagan bo'lsa, ular chaqaloq uchun xavfsiz deb hisoblashadi.[41]
Ko'plab ayollar "uyalash instinkti" deb nomlangan narsani boshdan kechirishlari ma'lum. Tug'ilishga kirishishdan oldin ayollar bir necha energiya haqida xabar berishadi.[41]

Xalq og'zaki ijodi uzoq vaqtdan beri aksariyat bolalar tunda yoki erta tongda dunyoga keladi va yaqinda o'tkazilgan (2018) tadqiqotlar AQShda buni to'g'ri deb topdi, ammo faqat uyda yoki shanba yoki yakshanba kunlari tug'ilgan bolalar uchun. Boshqa barcha tug'ilishlar, ehtimol, ertalab soat 8 dan peshingacha bo'lishi mumkin, bu rejalashtirilgan kesmalar odatda ertalab soat 8 da rejalashtirilganligini aks ettiradi, shu bilan tug'ruqdan tug'ilish ertalabki soatlarda ko'tarilib, soat 15 da eng yuqori ko'rsatkichga etgan. AQShda chaqaloqning tug'ilgan kuni uchun haftaning eng yaxshi kuni dushanba, so'ngra seshanba, rejalashtirilgan tug'ruq bilan ham bog'liq.[42][43]
Birinchi bosqich: yashirin faza
Yashirin bosqich, odatda, ayol muntazam ravishda qabul qiladigan nuqtadan boshlanishi bilan belgilanadi bachadonning qisqarishi.[44] Farqli o'laroq, Braxton Xiksning qisqarishi homiladorlikning 26 xaftaligidan boshlanishi mumkin bo'lgan va ba'zida "soxta mehnat" deb ataladigan kasılmalar, kamdan-kam uchraydi, tartibsiz va faqat engil krampni o'z ichiga oladi.[45]
Servikal bo'shliq ning ingichkalashi va cho'zilishi bachadon bo'yni va bachadon bo'yni kengayishi ning yopilish haftalarida sodir bo'ladi homiladorlik. Effacence odatda to'liq yoki deyarli tugaydi va kengayish yashirin fazaning oxiriga kelib taxminan 5 sm.[46] Servikal bo'shliq va kengayish darajasi qin tekshiruvi paytida sezilishi mumkin. Yashirin faza faol birinchi bosqich boshlanishi bilan tugaydi.
Birinchi bosqich: faol bosqich
Mehnatning faol bosqichi (yoki "birinchi bosqichning faol bosqichi", agar oldingi bosqich "birinchi bosqichning yashirin bosqichi" deb nomlansa) geografik jihatdan har xil ta'riflarga ega. Butunjahon sog'liqni saqlash tashkiloti faol birinchi bosqichni "bachadonning muntazam ravishda og'riqli qisqarishi, bachadon bo'yni bo'shatilishining asubstantiv darajasi va bachadon bo'yni 5 sm dan tez kengayishi bilan birinchi va keyingi mehnat uchun to'liq kengayishgacha bo'lgan davr" deb ta'riflaydi.[47] AQShda faol mehnat ta'rifi 3 sm dan 4 sm gacha, 5 sm ga o'zgartirildi bachadon bo'yni kengayishi ko'p bolali ayollar uchun, ilgari tug'gan onalar uchun va nullipar ayollar uchun 6 sm gacha, ilgari tug'ilmaganlar uchun.[48] Bu qin bilan tug'ilish tezligini oshirish maqsadida qilingan.[49]
Sog'liqni saqlash xodimlari, mehnatga layoqatli onaning tug'ruqdagi o'sishini bachadon bo'yni kengayishi, oqishi va stantsiyasini baholash uchun bachadon bo'yni tekshiruvini o'tkazish orqali baholashlari mumkin. Ushbu omillar Bishop ballari. Bishop balidan an muvaffaqiyatini bashorat qilish vositasi sifatida ham foydalanish mumkin mehnatni induktsiya qilish.
Chiqib ketish paytida bachadon bo'yni bachadonning pastki qismiga qo'shiladi. Qisish paytida bachadon mushaklari qisqarib, yuqori segment qisqaradi va pastki segment yuqoriga qarab, asta-sekin chiqarib yuboriladi.[iqtibos kerak ] Taqdim etilgan homila qismi pastga tushishga ruxsat beriladi. Bachadon bo'yni bola boshiga o'tishi uchun etarlicha kengayganida, to'laqonli kengayish, muddatiga etgan bola uchun 10 santimetr kengayish bilan amalga oshiriladi.
Yashirin birinchi bosqichning standart davomiyligi aniqlanmagan va bir ayoldan boshqasiga keng farq qilishi mumkin. Shu bilan birga, faol birinchi bosqichning davomiyligi (5 santimetrdan bachadon bo'yni to'liq kengayishigacha) odatda birinchi mehnatda 12 soatdan oshmaydi ("primiparae") va odatda keyingi ishlarda 10 soatdan oshmaydi ("multiparae"). [50]
Tug'ilish distosiyasi, shuningdek, "disfunktsional mehnat" yoki "rivojlanmaganlik" deb nomlanadi, bu og'ir mehnat yoki tug'ilishning g'ayritabiiy sekin rivojlanishi, bachadon bo'yni kengayishi yoki homila tushishining etishmasligi bilan bog'liq. 1955 yilda ishlab chiqarilgan Fridmanning egri chizig'i ko'p yillar davomida mehnat distosiyasini aniqlashda ishlatilgan. Ammo yaqinda o'tkazilgan tibbiy tadqiqotlar shuni ko'rsatadiki, Fridman egri chizig'i hozirda qo'llanilishi mumkin emas.[51][52]
Ikkinchi bosqich: xomilaning chiqarilishi

Chiqib ketish bosqichi bachadon bo'yni to'liq kengayganidan boshlanadi va bola tug'ilganda tugaydi. Bachadon bo'yni bosimi oshgani sayin, tos suyagi bosimi seziladi va shu bilan itarishni boshlash istagi paydo bo'ladi. Oddiy ikkinchi bosqichning boshida bosh tos suyagi bilan to'liq shug'ullanadi; boshning eng keng diametri tos suyagi teshigi. Keyin homila boshi tos suyagiga tushishni davom ettiradi, pubik kamon ostidan va qin orqali chiqib ketadi introitus (ochilish). Bunga o'xshash "tushirish" yoki itarish kabi qo'shimcha onalik harakatlari yordam beradi axlat. Xomila boshining qin teshigida paydo bo'lishi "toj kiyish" deb nomlanadi. Ayni paytda onada kuchli yonish yoki kuyish hissi paydo bo'ladi.
Qachon amniotik qop tug'ruq paytida yoki itarish paytida yorilib ketmagan bo'lsa, chaqaloq membranalari buzilmagan holda tug'ilishi mumkin. Bu "etkazib berish uz kaul ".
Chaqaloqni to'liq chiqarib tashlash, tug'ruqning ikkinchi bosqichi muvaffaqiyatli tugaganligidan dalolat beradi.
Ikkinchi bosqich bir ayoldan boshqasiga farq qiladi. Birinchi mehnatlarda tug'ilish odatda uch soat ichida tugaydi, keyingi mehnatlarda tug'ilish odatda ikki soat ichida tugaydi.[53] Uch soatdan ko'proq vaqt davom etadigan ikkinchi bosqichli mehnat o'z-o'zidan qin bilan tug'ilish tezligining pasayishi va infektsiyaning ko'payishi bilan bog'liq. perineal ko'z yoshlar va akusherlik qon ketishi, shuningdek, yangi tug'ilgan chaqaloqni intensiv davolash zarurati.[54]
Uchinchi bosqich: platsentani etkazib berish
Xomilaning chiqarilgandan so'ng, platsenta chiqarilgandan keyingigacha bo'lgan muddat deyiladi mehnatning uchinchi bosqichi yoki involution bosqichi. Plasentaning chiqarilishi bachadon devoridan fiziologik ajralish sifatida boshlanadi. Bolani tug'ruqdan platsentani to'liq chiqarib yuborishgacha bo'lgan o'rtacha vaqt 10-12 daqiqani tashkil qiladi, bu faol yoki kutilayotgan boshqaruv ishiga bog'liq.[55] Vaginal tug'ilishning 3 foizida uchinchi bosqichning davomiyligi 30 daqiqadan ko'proq va tashvish tug'diradi. saqlanib qolgan platsenta.[56]
Plasentani chiqarib yuborishni faol boshqarish mumkin yoki uni kutish bilan boshqarish mumkin, bu esa platsentani tibbiy yordamisiz chiqarib yuborishga imkon beradi. Faol boshqaruv - bu ma'muriyat uterotonik homila tug'ilgandan keyin bir daqiqa ichida dori, kindik ichakchasidagi tortilishi va asosiy platsenta tug'ilgandan keyin massaj, so'ngra bachadon massajini har 15 daqiqada ikki soat davomida bajarish.[57] Qo'shma bayonotda, Jahon Sog'liqni saqlash tashkiloti, Xalqaro ginekologiya va akusherlik federatsiyasi va Xalqaro doyalar konfederatsiyasi oldini olish uchun barcha qin bilan tug'ruqlarda tug'ruqning uchinchi bosqichini faol boshqarishni tavsiya eting tug'ruqdan keyingi qon ketish.[58][59][60]
Siqishni kechiktirish kindik ichakchasi kamida bir daqiqa yoki pulsatsiyani to'xtatguncha, bir necha daqiqa o'tishi mumkin, davolanish imkoniyati mavjud bo'lganda natijalar yaxshilanadi sariqlik agar u paydo bo'lsa. Ko'p yillar davomida kordonni kechiktirib kesish onaning tug'ilgandan keyin qon ketish xavfi tug'diradi, deb nomlangan tug'ruqdan keyingi qon ketish. Ammo yaqinda o'tkazilgan tekshiruv shuni ko'rsatdiki, sog'lom to'la tug'ilgan chaqaloqlarda kechiktirilgan simni kesish erta natijalarga olib keldi gemoglobin tug'ruqdan keyingi qon ketish darajasi o'zgarmasdan, tug'ilishdan olti oygacha konsentratsiya va tug'ilishning yuqori darajasi va temir zaxiralarining ko'payishi.[61][62]
To'rtinchi bosqich

"Tug'ilishning to'rtinchi bosqichi" - bu bola tug'ilgandan so'ng darhol boshlanib, taxminan olti hafta davom etadigan davr. Shartlar tug'ruqdan keyingi va tug'ruqdan keyingi ko'pincha ushbu davr uchun ishlatiladi.[63] Ayolning tanasi, shu jumladan gormonlar darajasi va bachadon hajmi, homilador bo'lmagan holatga qaytadi va yangi tug'ilgan chaqaloq onaning tanasidan tashqarida hayotga moslashadi. The Jahon Sog'liqni saqlash tashkiloti (JSST) tug'ruqdan keyingi davrni onalar va chaqaloqlar hayotidagi eng muhim va shu bilan birga beparvo qilingan bosqich deb ta'riflaydi; ko'pincha o'lim tug'ruqdan keyingi davrda sodir bo'ladi.[64]
Tug'ilgandan so'ng, agar onaning onasi bo'lsa epizyotomiya yoki ning yirtilishi perineum, u tikilgan. Bu, shuningdek, qabul qilish uchun maqbul vaqt uzoq muddatli qayta tiklanadigan kontratseptsiya (LARC), masalan kontratseptsiya vositasi yoki intrauterin vosita (IUD), ikkalasi ham tug'ruqdan keyin darhol ayol tug'ruq xonasida bo'lishi mumkin.[65][66] Onaning bachadon qisqarishi va uchun muntazam ravishda baholari bor asosiy balandlik,[67] Tug'ilgandan keyingi dastlabki 24 soat ichida qindan qon ketish, yurak urishi va qon bosimi va harorat. Siydikning birinchi o'tishi olti soat ichida hujjatlashtirilishi kerak.[64] Ortiqcha qon ketishini oldini olish uchun og'riq (hayz kramplariga o'xshash og'riqlar), bachadonning qisqarishi bir necha kun davom etadi. "Lokiya" deb nomlangan qindan bo'shatish bir necha hafta davom etishi mumkin; dastlab yorqin qizil rang, u asta-sekin pushti rangga aylanib, jigarrangga va nihoyat sariq yoki oq rangga aylanadi.[68] Ba'zi ayollar titroq yoki nazoratsiz epizodni boshdan kechirishadi tug'ruqdan keyingi sovuqlik, tug'ilgandan keyin.
Yaqin vaqtgacha kasalxonalarda tug'ilgan chaqaloqlar tug'ilgandan ko'p o'tmay onalaridan olib tashlangan va onaga faqat ovqatlanish vaqtida olib kelingan. Onalarga yangi tug'ilgan chaqaloqni bolalar bog'chasida xavfsizroq bo'lishlari va ajralish onaga ko'proq dam olishga ko'proq vaqt ajratishini aytishdi. O'zaro munosabatlarning o'zgarishi bilan, ba'zi shifoxonalarda "xonada yashash" opsiyasi mavjud bo'lib, unda bir muncha vaqtgacha kasalxonada o'tkazilgan muntazam muolajalar va kuzatuvlardan so'ng chaqaloq onaning xonasida bo'lishiga ruxsat berilishi mumkin. 2020 yildan boshlab xonada yashash odatiy amaliyotga aylandi.
Taxminan 2000 ta hokimiyat yangi tug'ilgan chaqaloqni tug'ruqdan keyingi odatdagi postnatal protsedura uchun onasiga qaytarilishidan oldin olib tashlash amaliyotini so'roq qila boshladi. Ba'zi rasmiylar teridan teriga erta aloqada bo'lish (yalang'och bolani onaning ko'kragiga qo'yish) onaga ham, chaqaloqqa ham foyda keltirishi mumkin deb taxmin qila boshladilar. Teridan-teriga tegishlgan samimiy aloqada namuna sifatida asosiy biologik ehtiyojlarni qondirishga olib keladigan neyroxatti-harakatlarni rag'batlantirishni ko'rsatadigan hayvonlarni o'rganish yordamida, agar mavjud bo'lsa, afzalliklarning erta teri bilan bog'liqligini baholash bo'yicha tadqiqotlar o'tkazildi. inson onalari va ularning chaqaloqlari uchun teriga tegish. 2011 yilgi tibbiy tekshiruvda mavjud tadqiqotlar ko'rib chiqildi va terining teriga erta aloqasi, ba'zan chaqirilganligi aniqlandi kenguru parvarishi, natijada yaxshilandi emizish natijalar, kardio-nafas olish barqarorligi va chaqaloq yig'lashining pasayishi.[69][70] 2016 yil Cochrane-ni ko'rib chiqish tug'ilish paytida terining teriga tegishi emizish ehtimoli va samaradorligini oshirishini aniqladi.[71]
2014 yildan boshlab, tug'ruqdan keyingi teridan teriga aloqani chaqaloqlarning farovonligi uchun mas'ul bo'lgan barcha yirik tashkilotlar, shu jumladan, Amerika Pediatriya Akademiyasi.[17] The Jahon Sog'liqni saqlash tashkiloti (JSST) ta'kidlashicha, "bola platsentadan sut emizishga xavfsiz tarzda o'tmaguncha, tug'ilish jarayoni tugamaydi". Vaginal tug'ilishdan keyin yangi tug'ilgan chaqaloqni onasi bilan teriga joylashtirilishi yoki sezaryen so'ng onasi hushyor va sezgir bo'lishi bilan har qanday muntazam muolajalarni kamida bir-ikki soatga qoldirishi tavsiya etiladi. JSST go'dak onasiga yaqin bo'lib qolganda, go'dakni har qanday dastlabki kuzatuvlarini amalga oshirish mumkin, deb ta'kidlaydi, chunki bola birinchi ovqatlanishidan oldin qisqa vaqt ajratish ham bog'lanish jarayonini buzishi mumkin. Ular qo'shimcha ravishda etkazib berishdan keyingi dastlabki kunlarda, ayniqsa, etkazib berishdan keyin biron sababga ko'ra uzilib qolgan bo'lsa, iloji boricha tez-tez teriga teriga tegib turishga maslahat beradi.[18] [19]
Mehnat induktsiyasi va elektektiv sezaryen bo'limi
Ko'p hollarda va ko'payib borayotgan chastotada tug'ish orqali erishiladi mehnatni induktsiya qilish yoki sezaryen bilan kesish. Mehnat induksiyasi - bu tug'ish va tug'ilishni rag'batlantiradigan jarayon yoki davolash. Ishni qo'zg'atish farmatsevtik yoki farmatsevtik bo'lmagan usullar bilan amalga oshirilishi mumkin. Induktsiyalar ko'pincha yoki bilan amalga oshiriladi prostaglandin yolg'iz dori-darmon bilan davolash yoki prostaglandin va tomir ichiga yuborish oksitotsin davolash ..[72]Sezaryen - bu olib tashlash yangi tug'ilgan qin bilan tug'ilish orqali emas, balki qorin bo'shlig'idagi jarrohlik kesma orqali.[73] 1996 yildan 2006 yilgacha AQShda tug'ruq bo'limlari bo'yicha tug'ilish 50 foizga o'sdi. 2011 yilda AQShda tug'ilishning 32,8 foizi sezaryen bilan tug'ildi.[73] 39-haftadan oldin tug'ruq va tug'ma sezaryen yangi tug'ilgan chaqaloq uchun ham, onaga ham zararli yoki foydasiz bo'lishi mumkin. Shu sababli, ko'plab ko'rsatmalar 39-haftadan oldin tibbiy talab qilinmaydigan tug'ruq va elektektiv sezaryenga qarshi tavsiya etiladi.[74] Qo'shma Shtatlarda 2012 yilda mehnatga jalb qilish darajasi 23,3 foizni tashkil etdi va 1990 yildan 2010 yilgacha ikki baravarga oshdi.[75][76] The Amerika akusher-ginekologlar Kongressi (ACOG) ko'rsatmalarida tug'ma tug'ruq induktsiyasini ko'rib chiqishda yangi tug'ilgan chaqaloqning optimal sog'lig'i uchun ona-homila holatini, bachadon bo'yni holatini va kamida 39 homiladorlik haftasini (to'liq muddatini) to'liq baholash tavsiya etiladi. Ushbu ko'rsatmalarga muvofiq quyidagi shartlar induksiya uchun ko'rsatma bo'lishi mumkin, jumladan:
- Abruptio platsentalari
- Chorioamnionit
- Isoimmunizatsiya kabi xomilalik murosaga olib keladi yangi tug'ilgan chaqaloqning gemolitik kasalligi yoki oligohidramnios
- Xomilalik o'lim
- Homiladorlik gipertenziyasi
- Kabi ona sharoitlari homiladorlik qandli diabet yoki surunkali buyrak kasalligi
- Preeklampsi yoki eklampsi
- Membranalarning erta yorilishi
- Postterm homiladorlik
İndüksiyon shuningdek logistik sabablarga ko'ra, masalan, kasalxonadan yoki psixosotsial sharoitlardan uzoqligi sababli ko'rib chiqiladi, ammo bu holatlarda homiladorlik davrini tasdiqlash kerak va xomilaning o'pkasining etukligi test orqali tasdiqlanishi kerak. ACOG, shuningdek, qo'zg'atilgan tug'ruq uchun kontrendikatsiyalar, shu jumladan o'z-o'zidan qin orqali etkazib berish bilan bir xil ekanligini ta'kidlaydi vasa previa, to'liq platsenta praevia, kindik ichakchasidagi prolapsus yoki faol oddiy jinsiy gerpes infektsiya.[77]
Menejment
Yetkazib berishga bir qator mutaxassislar yordam beradi, jumladan: akusherlar, oilaviy shifokorlar va doyalar. Xavfsiz homiladorlik uchun uchalasi ham shunga o'xshash natijalarga olib keladi.[79]
Tayyorgarlik
Tug'ruq paytida ovqatlanish yoki ichish doimiy munozaralar maydonidir. Ba'zilar, mehnatda ovqatlanish natijalarga zararli ta'sir ko'rsatmaydi, deb ta'kidlashsa ham,[80] Boshqalar homiladorlik paytida qizilo'ngachning bo'shashishi, bachadonning oshqozonga ko'tarilish bosimi va favqulodda tug'ruq paytida aspiratsiya hodisasi (yaqinda iste'mol qilingan oziq-ovqat mahsulotlariga bo'g'ilib qolish) xavfi borligidan xavotirda. favqulodda sezaryen paytida umumiy og'riqsizlantirish vositasi.[81] 2013 yil Cochrane-ni ko'rib chiqish yaxshi akusherlik behushligi bilan operatsiyaga muhtojligi past bo'lganlarda mehnat paytida ovqatlanish va ichishga ruxsat berishning zarari o'zgarmasligini aniqladi. Ular qo'shimcha ravishda tanovul qilmaslik och qorni borligini anglatmasligini yoki uning tarkibi u qadar kislotali emasligini tan olishadi. Shuning uchun ular "ayollar mehnatda ovqatlanish va ichish erkin bo'lishi kerak, yoki xohlaganicha bo'lmasligi kerak" degan xulosaga kelishadi.[82]
Bir vaqtning o'zida sochni oldirish qin atrofidagi joy, soch olib tashlash infektsiya xavfini kamaytiradi degan ishonch tufayli keng tarqalgan amaliyot edi epizyotomiya (vaginal kirishni kattalashtirish uchun jarrohlik yo'li bilan kesish) osonroq va asbob bilan etkazib berishda yordam berdi. Hozirgi kunda bu kamroq tarqalgan, garchi ba'zi mamlakatlarda odatiy protsedura bo'lsa ham, muntazam ravishda ko'rib chiqishda sochingizni olishni tavsiya qiladigan dalillar topilmadi.[83] Yon ta'siri keyinchalik paydo bo'ladi, shu jumladan tirnash xususiyati, qizarish va ustara ustidagi bir nechta yuzaki chizish. Infektsiyani oldini olish uchun yana bir harakat antiseptikdan foydalanish bo'ldi xlorheksidin yoki providon-yod eritmasi qin ichida. Xlorheksidin bilan foyda keltiradigan dalillar yo'q.[84] Sezaryen kesimida providon-yod bilan kamaygan xavf aniqlanadi.[85]
Forseps yoki vakuum yordamida etkazib berish
Yordam bilan tug'ilish har 8 tug'ilishning 1tasida qo'llaniladi va agar ona yoki bola qinida tug'ilish paytida xavf ostida bo'lsa, kerak bo'lishi mumkin. Amaldagi usullar nomlanadi akusherlik forsepslari qazib olish va vakuum ekstrakti, ventouse ekstraktsiyasi deb ham ataladi. To'g'ri bajarilgan bo'lsa, ularning ikkalasi ham vakuumga emas, balki forsepslarga afzallik berishlari bilan xavfsizdir va ikkalasi ham kutilmagan C-bo'limidan afzalroqdir. Xavfsiz deb hisoblansa-da, ona uchun ba'zi xavflar orasida qinning yirtilishi, shu jumladan anus yoki rektumning mushaklari yoki devorlarini o'z ichiga oladigan katta qin yoshi paydo bo'lishi ehtimoli mavjud. Oyoqlarda yoki tosda qon pıhtılarının paydo bo'lishi xavfi yuqori - pıhtılaşmaya yo'l qo'ymaslik uchun trombga qarshi paypoq yoki dori-darmon buyurilishi mumkin. Siydik chiqarishning buzilishi Tug'ilgandan keyin g'ayrioddiy emas, lekin asbob etkazib berilgandan keyin tez-tez uchraydi. Muayyan mashqlar va fizioterapiya vaziyatni yaxshilashga yordam beradi.[86]
Og'riqni nazorat qilish
Farmatsevtik bo'lmagan
Ba'zi ayollar qochishni afzal ko'rishadi og'riq qoldiruvchi tug'ruq paytida dorilar. Psixologik tayyorgarlik foydali bo'lishi mumkin. Dam olish texnikasi, suvga cho'mish, massaj va akupunktur og'riqni engillashtirishi mumkin. Akupunktur va gevşeme kerakli sezaryen sonini kamaytirishi aniqlandi.[87] Suvga cho'mish tug'ruqning birinchi bosqichida og'riqni engillashtirishi va behushlik talabini kamaytirishi va tug'ilish muddatini qisqartirishi aniqlandi, ammo tug'ilish paytida suvga cho'mish xavfsizligi va samaradorligi, suvda tug'ilish, onalik yoki homila foydasi aniqlanmagan yoki bog'liq emas.[88]
Aksariyat ayollar mehnat va tug'ilish paytida ularni qo'llab-quvvatlaydigan odamga ega bo'lishni yaxshi ko'radilar; masalan, doya, hamshira yoki doula; yoki chaqaloqning otasi, oila a'zosi yoki yaqin do'sti kabi oddiy odam. Tadqiqotlar shuni ko'rsatdiki, tug'ruq paytida va tug'ruq paytida doimiy qo'llab-quvvatlash dori-darmonlarga va sezaryen bilan yoki operativ qin bilan tug'ilishga bo'lgan ehtiyojni kamaytiradi va natijada yaxshilanadi Apgar ballari go'dak uchun[89][90]
Farmatsevtika
Og'riqni nazorat qilish bo'yicha turli xil chora-tadbirlar ayol va uning chaqalog'ida turli darajadagi muvaffaqiyat va yon ta'sirga ega. Evropaning ayrim mamlakatlarida shifokorlar odatda nafas olishni buyuradilar azot oksidi og'riqni nazorat qilish uchun gaz, ayniqsa 53% azot oksidi, 47% kislorod sifatida tanilgan Entonoks; Buyuk Britaniyada doyalar ushbu gazdan shifokorning retseptisiz foydalanishlari mumkin.[91] Opioidlar kabi fentanil ishlatilishi mumkin, ammo tug'ilishga juda yaqin bo'lsa, go'dakda nafas olish tushkunligi xavfi mavjud.[iqtibos kerak ]
Kasalxonalarda mashhur tibbiy og'riqni nazorat qilish mintaqaviy anestezikani o'z ichiga oladi epidurallar (EDA) va o'murtqa behushlik. Epidural analjeziya odatda og'riqni engillashtiradigan xavfsiz va samarali usuldir, ammo u uzoqroq mehnat qilish, ko'proq operativ aralashuv (xususan, asbob etkazib berish) va narxning oshishi bilan bog'liq.[92] Shu bilan birga, yaqinda (2017) Cochrane-ning tekshiruvi shuni ko'rsatadiki, yangi epidural texnikasi ish vaqtiga va asboblardan foydalanishga yoki kesma etkazib berishga bo'lgan ehtiyojga ta'sir qilmaydi.[93] Odatda, epidurallarsiz ayollar uchun og'riq va stress gormonlari butun mehnat davomida ko'payadi, og'riq, qo'rquv va stress gormonlari epidural analjeziya yuborilgandan keyin kamayadi, ammo keyin yana ko'tariladi.[94]Epidural orqali yuboriladigan dori platsentadan o'tib, homilaning qon oqimiga tushishi mumkin.[95] Epidural analjeziya sezaryen bilan kasallanish xavfiga statistik jihatdan sezilarli ta'sir ko'rsatmaydi va Apgar ballari bilan aniqlangan yangi tug'ilgan holatga darhol ta'sir ko'rsatmaydi.[93]
Kattalashtirish

Kattalashtirish - bu tug'ruq boshlangandan keyin bachadonni qisqarish intensivligi va davomiyligini oshirish uchun rag'batlantirish jarayoni. Bachadonning qisqarishi juda zaif deb baholanganda, tug'ilishning sekin o'sishini (distosiya) davolash uchun ko'paytirishning bir necha usullari qo'llaniladi. Oksitotsin qin bilan etkazib berish tezligini oshirish uchun ishlatiladigan eng keng tarqalgan usul.[96] Jahon sog'liqni saqlash tashkiloti uni yakka o'zi yoki birga ishlatishni tavsiya qiladi amniotomiya (amniotik membrananing yorilishi), ammo agar zararni oldini olish kerak bo'lsa, mehnatning to'g'ri ketmasligi to'g'ri tasdiqlanganidan keyingina foydalanilishi lozimligini maslahat beradi. JSST foydalanishni tavsiya etmaydi antispazmodik tug'ilishning kechikishini oldini olish uchun vositalar.[97]
Epiziotomiya
Bir necha yillar davomida epizyotomiya Vaginal ko'z yoshlarini oldini olish va tabiiy ko'z yoshidan ko'ra yaxshiroq davolanishga yordam beradi deb o'ylashgan. Perineal ko'z yoshlari bolaning boshi o'tishi bilan qinning ochilishida paydo bo'lishi mumkin, ayniqsa, bola tezda pastga tushsa. Ko'z yoshlar o'z ichiga olishi mumkin perineal teri yoki mushaklarga va anal sfinkter va anusga cho'ziladi. Bir vaqtlar keng tarqalgan bo'lib, endi ular umuman kerak emas deb tan olindi.[15] Zarur bo'lganda, akusher yoki akusher perineumni jarrohlik yo'li bilan kesib, tiklanishi qiyin bo'lgan qattiq ko'z yoshlarini oldini oladi. 2017 yilgi Cochrane tekshiruvi epiziotomiyani zarurat bo'yicha (cheklovchi) muntazam epizyotomiya bilan taqqoslab, ona va bola uchun mumkin bo'lgan foyda va zararni aniqladi. Tadqiqot shuni ko'rsatdiki, cheklovchi epizyotomiya siyosati odatdagi epizyotomiya bilan taqqoslaganda bir qator afzalliklarga ega. Tug'ilgandan keyin og'riq, siydik chiqarmaslik, og'riqli jinsiy aloqa yoki og'ir vaginal / perineal travma bilan farq qilmasdan, etti kun davomida ayollar kamroq perineal travma, kamroq perineal travma, kamroq tikuv va kamroq davolovchi asoratlarni boshdan kechirdilar.[98]
Ko'p tug'ilish
Hollarda a birinchi taqdimot boshi birinchi egizak, egizak ko'pincha qin orqali tug'ilishi mumkin. Ba'zi hollarda egizak tug'ish katta tug'ruq xonasida yoki operatsiya teatrida amalga oshiriladi, masalan, asorat bo'lsa.
- Ikkala egizak ham qindan tug'iladi - bu ikkalasi ham birinchi bo'lib bosh yoki birinchi bo'lib bosh, ikkinchisi kaltaklangan va / yoki forseps / ventouz etkazib berishda yordam beradigan joyda sodir bo'lishi mumkin.
- Bittasi qin bilan, ikkinchisi sezaryen bilan tug'ilgan.
- Agar egizaklar tananing biron bir qismida birlashtirilsa - chaqiriladi birlashtirilgan egizaklar, etkazib berish asosan sezaryen bilan amalga oshiriladi.
Qo'llab-quvvatlash

Obstetric care frequently subjects women to institutional routines, which may have adverse effects on the progress of labour. Supportive care during labour may involve emotional support, comfort measures, and information and advocacy which may promote the physical process of labour as well as women's feelings of control and competence, thus reducing the need for obstetric intervention. The continuous support may be provided either by hospital staff such as nurses or midwives, doulas, or by companions of the woman's choice from her social network. A 2015 Cochrane review examined debriefing interventions for women who perceived childbirth as being traumatic but failed to find any evidence to support routine debriefing as a needed intervention after childbirth.[99] There is increasing evidence to show that the participation of the child's father in the birth leads to better birth and also post-birth outcomes, providing the father does not exhibit excessive anxiety.[100]
Continuous labour support may help women to give birth spontaneously, i.e. without caesarean or vacuum or forceps, with slightly shorter labours, and to have more positive feelings regarding their experience of giving birth. Continuous labour support may also reduce women's use of pain medication during labour and reduce the risk of babies having low five-minute Agpar scores.[101]
Fetal monitoring
External monitoring
Uchun monitoring of the fetus during childbirth, a simple pinard stethoscope yoki doppler fetal monitor ("doptone ") can be used.A method of external (noninvasive) fetal monitoring (EFM) during childbirth is cardiotocography (CTG), using a cardiotocograph that consists of two sensors: The yurak (cardio) sensor is an ultrasonic sensor, a ga o'xshash Doppler fetal monitor, that continuously emits ultrasound and detects motion of the fetal heart by the characteristic of the reflected sound. The pressure-sensitive qisqarish transducer, called a tocodynamometer (toco) has a flat area that is fixated to the skin by a band around the belly. The pressure required to flatten a section of the wall correlates with the internal pressure, thereby providing an estimate of contraction.[102]Monitoring with a cardiotocograph can either be intermittent or continuous.[103] The Jahon Sog'liqni saqlash tashkiloti (WHO) advises that for healthy women undergoing spontaneous labour continuous cardiotocography is not recommended for assessment of fetal well-being. The WHO states: "In countries and settings where continuous CTG is used defensively to protect against litigation, all stakeholders should be made aware that this practice is not evidence-based and does not improve birth outcomes."[104]
Internal monitoring
A mother's water has to break before internal (invasive) monitoring can be used. More invasive monitoring can involve a fetal scalp electrode to give an additional measure of fetal heart activity, and/or intrauterine pressure catheter (IUPC). It can also involve fetal scalp pH testing.
Asoratlar


Per figures retrieved in 2015, since 1990 there has been a 44 per cent decline in the maternal death rate. However, according to 2015 figures 830 women die every day from causes related to pregnancy or childbirth and for every woman who dies, 20 or 30 encounter injuries, infections or disabilities. Most of these deaths and injuries are preventable.[106][107]
In 2008, noting that each year more than 100,000 women die of complications of pregnancy and childbirth and at least seven million experience serious health problems while 50 million more have adverse health consequences after childbirth, the Jahon Sog'liqni saqlash tashkiloti (WHO) has urged midwife training to strengthen maternal and newborn health services. To support the upgrading of midwifery skills the WHO established a midwife training program, Action for Safe Motherhood.[5]
The rising maternal death rate in the US is of concern. In 1990 the US ranked 12th of the 14 developed countries that were analyzed. However, since that time the rates of every country have steadily continued to improve while the US rate has spiked dramatically. While every other developed nation of the 14 analyzed in 1990 shows a 2017 death rate of less than 10 deaths per every 100,000 live births, the US rate has risen to 26.4. By comparison, the United Kingdom ranks second highest at 9.2 and Finland is the safest at 3.8.[108] Furthermore, for every one of the 700 to 900 US woman who die each year during pregnancy or childbirth, 70 experience significant complications such as hemorrhage and organ failure, totaling more than one percent of all births.[109]
Compared to other developed nations, the United States also has high infant mortality rates. The Trust for America's Health reports that as of 2011, about one-third of American births have some complications; many are directly related to the mother's health including increasing rates of obesity, type 2 diabetes, and physical inactivity. The U.S. Centers for Disease Control and Prevention (CDC) has led an initiative to improve woman's health previous to conception in an effort to improve both neonatal and maternal death rates.[110]
Labour and delivery complications
To'siq qilingan mehnat
The second stage of labour may be delayed or lengthy due to poor or uncoordinated uterine action, an abnormal uterine position such as kam yoki elka distosiyasi, and cephalopelvic disproportion (a small pelvis or large infant). Prolonged labour may result in maternal exhaustion, fetal distress, and other complications including akusherlik fistula.[111]
Eklampsi
Eclampsia is the onset of seizures (convulsions) in a woman with pre-eclampsia. Pre-eclampsia is a disorder of pregnancy in which there is high blood pressure and either large amounts of protein in the urine or other organ dysfunction. Pre-eclampsia is routinely screened for during prenatal care. Onset may be before, during, or rarely, after delivery. Around one percent of women with eclampsia die.
Onaning asoratlari
A puerperal disorder or postpartum disorder is a complication which presents primarily during the puerperium, or postpartum period. The postpartum period can be divided into three distinct stages; the initial or acute phase, six to 12 hours after childbirth; subacute postpartum period, which lasts two to six weeks, and the delayed postpartum period, which can last up to six months. In the subacute postpartum period, 87% to 94% of women report at least one health problem.[112][113] Long term health problems (persisting after the delayed postpartum period) are reported by 31 percent of women.[114]
Postpartum bleeding
Postpartum bleeding is the leading cause of death of birthing mothers in the world, especially in the developing world. Globally it occurs about 8.7 million times and results in 44,000 to 86,000 deaths per year. Uterine atony, the inability of the uterus to contract, is the most common cause of postpartum bleeding. Following delivery of the placenta, the uterus is left with a large area of open blood vessels which must be constricted to avoid blood loss. Retained placental tissue and infection may contribute to uterine atony. Heavy blood loss leads to gipovolemik shok, insufficient perfusion of vital organs and death if not rapidly treated.
Postpartum infections
Postpartum infections, also known as childbed fever and puerperal fever, are any bacterial infections of the reproductive tract following childbirth or miscarriage. Signs and symptoms usually include a fever greater than 38.0 °C (100.4 °F), chills, lower abdominal pain, and possibly bad-smelling vaginal discharge. The infection usually occurs after the first 24 hours and within the first ten days following delivery. Infection remains a major cause of maternal deaths and morbidity in the developing world. Ishi Ignaz Semmelveys was seminal in the pathophysiology and treatment of childbed fever and his work saved many lives.
Psychological complications
Childbirth can be an intense event and strong emotions, both positive and negative, can be brought to the surface. Abnormal and persistent fear of childbirth is known as tokophobia. The prevalence of fear of childbirth around the world ranges between 4–25%, with 3–7% of pregnant women having clinical fear of childbirth.[115][116]
Most new mothers may experience mild feelings of unhappiness and worry after giving birth. Babies require a lot of care, so it is normal for mothers to be worried about, or tired from, providing that care. The feelings, often termed the "baby blues", affect up to 80 percent of mothers. They are somewhat mild, last a week or two, and usually go away on their own.[117]
Tug'ilgandan keyingi depressiya is different from the "baby blues". With postpartum depression, feelings of sadness and anxiety can be extreme and might interfere with a woman's ability to care for herself or her family. Because of the severity of the symptoms, postpartum depression usually requires treatment. The condition, which occurs in nearly 15 percent of births, may begin shortly before or any time after childbirth, but commonly begins between a week and a month after delivery.[117]
Childbirth-related posttraumatic stress disorder is a psychological disorder that can develop in women who have recently given birth.[118][119][120] Causes include issues such as an emergency C-section, preterm labour, inadequate care during labour, lack of social support following childbirth, and others. Examples of symptoms include intrusive symptoms, orqaga qaytish va kabuslar, as well as symptoms of avoidance (shu jumladan amneziya for the whole or parts of the event), problems in developing a mother-child attachment, and others similar to those commonly experienced in travmatik stress buzilishi (TSSB). Many women who are experiencing symptoms of PTSD after childbirth are misdiagnosed with postpartum depression or adjustment disorders. These diagnoses can lead to inadequate treatment.[121]
Tug'ilgandan keyingi psixoz kamdan-kam uchraydi psychiatric emergency in which symptoms of high mood and racing thoughts (mani ), depression, severe confusion, loss of inhibition, paranoia, hallucinations and delusions set in, beginning suddenly in the first two weeks after childbirth. The symptoms vary and can change quickly.[122] It usually requires hospitalization. The most severe symptoms last from two to 12 weeks, and recovery takes six months to a year.[122]
Fetal complications

Five causes make up about 80 percent of newborn deaths. They include prematurity and low-birth-weight, infections, lack of oxygen at birth, and trauma during birth.[24]
Tug'ilish
Stillbirth is typically defined as homila death at or after 20 to 28 weeks of pregnancy.[123][124] It results in a baby born without signs of life.[124]
Worldwide prevention of most stillbirths is possible with improved health systems.[124][125] About half of stillbirths occur during childbirth, with this being more common in the rivojlanmoqda dan rivojlangan dunyo.[124] Otherwise depending on how far along the pregnancy is, medications may be used to start labor or a type of surgery known as dilation and evacuation may be carried out.[126] Following a stillbirth, women are at higher risk of another one; however, most subsequent pregnancies do not have similar problems.[127]
Worldwide in 2015 there were about 2.6 million stillbirths that occurred after 28 weeks of pregnancy (about 1 for every 45 births).[124][128] They occur most commonly in the developing world, particularly Janubiy Osiyo va Afrikaning Sahroi osti qismi.[124] In the United States for every 167 births there is one stillbirth.[128] Stillbirth rates have declined, though more slowly since the 2000s.[129]
Erta tug'ilish
Preterm birth is the birth of an infant at fewer than 37 weeks homiladorlik davri. It is estimated that one in 10 babies are born prematurely. Premature birth is the leading cause of death in children under five years of age though many that survive experience disabilities including learning defects and visual and hearing problems. Causes for early birth may be unknown or may be related to certain chronic conditions such as diabetes, infections, and other known causes. The World Health Organization has developed guidelines with recommendations to improve the chances of survival and health outcomes for preterm infants.[130]
Neonatal infektsiya

Newborns are prone to infection in the first month of life. The organism S. agalactiae (Group B Streptococcus) or (GBS) is most often the cause of these occasionally fatal infections. The baby contracts the infection from the mother during labor. In 2014 it was estimated that about one in 2000 newborn babies have GBS bacterial infections within the first week of life, usually evident as respiratory disease, general sepsis, yoki meningit.[132]
Untreated jinsiy yo'l bilan yuqadigan infektsiyalar (STIs) are associated with tug'ma and infections in newborn babies, particularly in the areas where rates of infection remain high. The majority of STIs have no symptoms or only mild symptoms that may not be recognized. Mortality rates resulting from some infections may be high, for example the overall perinatal mortality rate associated with untreated syphilis is 30 percent.[133]
Perinatal asphyxia
Perinatal asphyxia is the medical condition resulting from deprivation of oxygen to a newborn infant that lasts long enough during the birth process to cause physical harm, usually to the brain. Hypoxic damage can occur to most of the infant's organs (yurak, o'pka, jigar, ichak, buyraklar ), lekin miya shikastlanishi is of most concern and perhaps the least likely to quickly or completely heal.[134]
Mechanical fetal injury
Risk factors for fetal birth injury include fetal macrosomia (big baby), maternal obesity, the need for instrumental delivery, and an inexperienced attendant. Specific situations that can contribute to birth injury include breech presentation and elka distosiyasi. Most fetal birth injuries resolve without long term harm, but brachial plexus injury olib kelishi mumkin Erb's palsy yoki Klumpke's paralysis.[135]
Tarix
The process of childbirth in Western society has evolved significantly over the years.
Role of males
Historically women have been attended and supported by other women during labour and birth. Midwife training in European cities began in the 1400s, but rural women were usually assisted by female family or friends.[136] However, it was not simply a ladies' social bonding event as some historians have portrayed - fear and pain often filled the atmosphere, as death during childbirth was a common occurrence.[137] In the United States, before the 1950s the husband would not be in the birthing room. It did not matter if it was a home birth; the husband was waiting downstairs or in another room in the home. If it was in a hospital then the husband was in the waiting room.[138] Fathers were only permitted in the room if the life of the mother or baby was severely at-risk. In 1522, a German physician was sentenced to death for sneaking into a delivery room dressed as a woman.[136]
Ironically, the majority of guidebooks related to pregnancy and childbirth were written by men who had never been involved in the birthing process. A Greek physician, Soranus of Ephesus, wrote a book about obstetrics and gynecology in the second century, which was referenced for the next thousand years. The book contained endless home remedies for pregnancy and childbirth, many of which would be considered heinous by modern women and medical professionals.[136]
Both preterm and full term infants benefit from skin to skin contact, sometimes called Kangaroo care, immediately following birth and for the first few weeks of life. Recently some fathers have also begun to hold their newborns skin to skin as well. The new baby is familiar with the father's voice and it is believed that contact with the father helps the infant to stabilize and promotes father to infant bonding. If the infant's mother had a caesarean birth, the father can hold their baby in skin-to-skin contact while the mother recovers from the anesthetic.[139]
Kasalxonalar
Historically, most women gave birth at home without emergency medical care available. In the early days of hospitalization of childbirth, a 17th-century maternity ward in Paris was incredibly congested, with up to five pregnant women sharing one bed. At this hospital, one in five women died during the birthing process.[136] At the onset of the Sanoat inqilobi, giving birth at home became more difficult due to congested living spaces and dirty living conditions. That drove urban and lower-class women to newly-available hospitals, while wealthy and middle-class women continued to labor at home.[140] Consequently, wealthier women experienced lower maternal mortality rates than those of a lower social class.[141] Throughout the 1900s there was an increasing availability of hospitals, and more women began going into the hospital for labor and delivery.[142] In the United States, 5% of women gave birth in hospitals in 1900. By 1930, 50% of all women and 75% of urban-dwelling women delivered in hospitals.[136] By 1960, this number increased to 96%.[137] By the 1970s, home birth rates fell to approximately 1%.[143] In the United States, the middle classes were especially receptive to the medicalization of childbirth, which promised a safer and less painful labor.[142]
Accompanied by the shift from home to hospital was the shift from midwife to physician. Male physicians began to replace female midwives in Europe and the United States in the 1700s. The rise in status and popularity of this new position was accompanied by a drop in status for midwives. By the 1800s, affluent families were primarily calling male doctors to assist with their deliveries, and female midwives were seen as a resource for women who could not afford better care. That completely removed women from assisting in labor, as only men were eligible to become doctors at the time. Additionally, it privatized the birthing process as family members and friends were often banned from the delivery room.
There was opposition to the change from both progressive feminists and religious conservatives. The feminists were concerned about job security for a role that had traditionally been held by women. The conservatives argued that it was immoral for a woman to be exposed in such a way in front of a man. For that reason, many male obstetricians performed deliveries in dark rooms or with their patient fully covered with a drape.
Dori-darmon
The use of pain medication in labor has been a controversial issue for hundreds of years. A Scottish woman was burned at the stake in 1591 for requesting pain relief in the delivery of twins. Medication became more acceptable in 1852, when Queen Victoria used chloroform as pain relief during labor. Dan foydalanish morfin va scopolamine, shuningdek, nomi bilan tanilgan "twilight sleep," was first used in Germany and popularized by German physicians Bernard Kronig and Karl Gauss. This concoction offered minor pain relief but mostly allowed women to completely forget the entire delivery process. Under twilight sleep, mothers were often blindfolded and restrained as they experienced the immense pain of childbirth. The cocktail came with severe side effects, such as decreased uterine contractions and altered mental state. Additionally, babies delivered with the use of childbirth drugs often experienced temporarily-ceased breathing. The feminist movement in the United States openly and actively supported the use of twilight sleep, which was introduced to the country in 1914. Some physicians, many of whom had been using painkillers for the past fifty years, including opium, cocaine, and quinine, embraced the new drug. Others were rightfully hesitant.[136]
Caesarean sections
While forceps have gone through periods of high popularity, today they are only used in approximately 10 percent of deliveries. The caesarean section (or C-section) has become the more popular solution for difficult deliveries. In 2005, one-third of babies were born via C-section. Historically, surgical delivery was a last-resort method of extracting a baby from its deceased or dying mother. There are many conflicting stories of the first successful C-section in which both mother and baby survived. It is, however, known that the procedure had been attempted for hundreds of years before it became accepted in the beginning of the twentieth century.[136]
Tabiiy tug'ilish
The re-emergence of "natural childbirth" began in Europe and was adopted by some in the US as early as the late 1940s. Early supporters believed that the drugs used during deliveries interfered with "happy childbirth" and could negatively impact the newborn's "emotional wellbeing." By the 1970s, the call for natural childbirth was spread nationwide, in conjunction with the second-wave of the feminist movement.[136] While it is still most common for American women to deliver in the hospital, supporters of natural birth still widely exist, especially in the UK where midwife-assisted home births have gained popularity in recent years.[143]
Onalar o'limi

Childbirth statistics in the US before 1915 were not recorded, but moving forward, the US has had historically poor maternal mortality rates in comparison to other developed countries. There is more reliable data on maternal mortality from Britain from 1880 onward. Outcomes for mothers in childbirth were especially poor before 1930 because of high rates of puerperal fever.[141] Gacha mikroblar nazariyasi was accepted in the mid-1800s, it was assumed that puerperal fever was either caused by a variety of sources, including the leakage of breast milk into the body and anxiety, rather than by a pathogen that was transmitted by the dirty hands and tools of doctors. That misconception was likely responsible for the high prevalence of puerperal fever.[136] The home births facilitated by trained midwives produced the best outcomes from 1880 to 1930 in the US and Europe, whereas physician-facilitated hospital births produced the worst. The change in trend of maternal mortality can be attributed with the widespread use of sulfanilamidlar, along with the progression of medical technology, more extensive physician training, and less medical interference with normal deliveries.[141]
Jamiyat va madaniyat
Xarajatlar

According to a 2013 analysis performed commissioned by the New York Times and performed by Truven Healthcare Analytics, the cost of childbirth varies dramatically by country. In the United States the average amount actually paid by insurance companies or other payers in 2012 averaged $9,775 for an uncomplicated conventional delivery and $15,041 for a caesarean birth.[144] The aggregate charges of healthcare facilities for four million annual births in the United States was estimated at over $50 billion. The summed cost of prenatal care, childbirth, and newborn care came to $30,000 for a vaginal delivery and $50,000 for a caesarian section.
In the United States, childbirth hospital stays have some of the lowest ICU utilizations. Vaginal delivery with and without complicating diagnoses and caesarean section with and without comorbidities or major comorbidities account for four of the 15 types of hospital stays with low rates of ICU utilization (where less than 20% of visits were admitted to the ICU). During stays with ICU services, approximately 20% of costs were attributable to the ICU.[145]
A 2013 study found varying costs by facility for childbirth expenses in California, varying from $3,296 to $37,227 for a vaginal birth and from $8,312 to $70,908 for a caesarean birth.[146]
Beginning in 2014, the Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti began recommending that many women give birth at home under the care of a midwife rather than an obstetrician, citing lower expenses and better healthcare outcomes.[147] [148] The median cost associated with home birth was estimated to be about $1,500 vs. about $2,500 in hospital.[149]
Manzil
Childbirth routinely occurs in hospitals in many rivojlangan mamlakatlar. Before the 20th century and in some countries to the present day, such as Nederlandiya, it has more typically occurred at home.[150]
In rural and remote communities of many countries, hospitalized childbirth may not be readily available or the best option. Maternal evacuation is the predominant risk management method for assisting mothers in these communities.[151] Maternal evacuation is the process of relocating pregnant women in remote communities to deliver their babies in a nearby urban hospital setting.[151] This practice is common in Indigenous Inuit and Northern Manitoban communities in Kanada shu qatorda; shu bilan birga Avstraliyalik aboriginal communities. There has been research considering the negative effects of maternal evacuation due to a lack of social support provided to these women. These negative effects include an increase in maternal newborn complications and postpartum depression, and decreased breastfeeding rates.[151]
The exact location in which childbirth takes place is an important factor in determining nationality, in particular for birth aboard aircraft and ships.
Imkoniyatlar
Following are facilities that are particularly intended to house women during childbirth:
- A labour ward, shuningdek, a deb nomlangan delivery ward yoki labour and delivery, is generally a department of a hospital that focuses on providing Sog'liqni saqlash to women and their children during childbirth. It is generally closely linked to the hospital's neonatal intensiv terapiya bo'limi va / yoki obstetric surgery unit if present. A tug'ruq bo'limi yoki maternity unit may include facilities both for childbirth and for tug'ruqdan keyingi rest and observation of mothers in normal as well as complicated cases.
- A maternity hospital is a hospital that specializes in caring for women while they are pregnant and during childbirth and provide care for newborn babies,
- A tug'ish markazi generally presents a simulated home-like environment. Birthing centers may be located on hospital grounds or "free standing" (i.e., not hospital-affiliated).
- In addition, it is possible to have a home birth, usually with the assist of a midwife. However, some women choose to give birth at home without any professionals present, termed an unassisted childbirth.
Associated occupations

Different categories of tug'ilganlar may provide support and care during pregnancy and childbirth, although there are important differences across categories based on professional training and skills, practice regulations, and the nature of care delivered. Many of these occupations are highly professionalised, but other roles exist on a less formal basis.
"Childbirth educators" are instructors who aim to teach pregnant women and their partners about the nature of pregnancy, labour signs and stages, techniques for giving birth, breastfeeding and newborn baby care. Training for this role can be found in hospital settings or through independent certifying organizations. Each organization teaches its own curriculum and each emphasizes different techniques. The Lamaze texnikasi is one well-known example.
Doulas are assistants who support mothers during pregnancy, labour, birth, and postpartum. They are not medical attendants; rather, they provide emotional support and non-medical pain relief for women during labour. Like childbirth educators and other unlicensed assistive personnel, certification to become a doula is not compulsory, thus, anyone can call themself a doula or a childbirth educator.
Confinement nannies are individuals who are employed to provide assistance and stay with the mothers at their home after childbirth. They are usually experienced mothers who took courses on how to take care of mothers and newborn babies.[152]
Doyalar are autonomous practitioners who provide basic and emergency health care before, during and after pregnancy and childbirth, generally to women with low-risk pregnancies. Midwives are trained to assist during labour and birth, either through direct-entry or nurse-midwifery education programs. Jurisdictions where midwifery is a regulated profession will typically have a registering and disciplinary body for quality control, such as the American Midwifery Certification Board in the United States,[153] the College of Midwives of British Columbia in Canada[154][155] yoki Nursing and Midwifery Council Buyuk Britaniyada.[156][157]
In the past, midwifery played a crucial role in childbirth throughout most indigenous societies. Although western civilizations attempted to assimilate their birthing technologies into certain indigenous societies, like Kaplumbağa oroli, and get rid of the midwifery, the National Aboriginal Council of Midwives brought back the cultural ideas and midwifery that were once associated with indigenous birthing.[158]
In jurisdictions where midwifery is not a regulated profession, traditional birth attendants, also known as traditional or lay midwives, may assist women during childbirth, although they do not typically receive formal health care education and training.
Medical doctors who practice in the field of childbirth include categorically specialized akusherlar, oilaviy amaliyotchilar va umumiy amaliyot shifokorlari whose training, skills and practices include obstetrics, and in some contexts umumiy jarrohlar. These physicians and surgeons variously provide care across the whole spectrum of normal and abnormal births and pathological labour conditions. Categorically specialized obstetricians are qualified jarrohlar, so they can undertake surgical procedures relating to childbirth. Some family practitioners or general practitioners also perform obstetrical surgery. Obstetrical procedures include cesarean sections, epizyotomiyalar, and assisted delivery. Categorical specialists in obstetrics are commonly trained in both akusherlik va ginekologiya (OB/GYN), and may provide other medical and surgical gynecological care, and may incorporate more general, well-woman, birlamchi tibbiy yordam elements in their practices. Maternal-fetal medicine specialists are obstetrician/gynecologists subspecialized in managing and treating high-risk pregnancy and delivery.
Anaesthetists yoki anesthesiologists are medical doctors who specialise in pain relief and the use of drugs to facilitate surgery and other painful procedures. They may contribute to the care of a woman in labour by performing an epidural or by providing behushlik (ko'pincha spinal anaesthesia ) uchun Kesariy qism yoki forceps delivery. They are experts in pain management during childbirth.
Obstetric nurses assist midwives, doctors, women, and babies before, during, and after the birth process, in the hospital system. They hold various nursing certifications and typically undergo additional obstetric training in addition to standard nursing training.
Feldsherlar are healthcare providers that are able to provide emergency care to both the mother and infant during and after delivery using a wide range of medications and tools on an ambulance. They are capable of delivering babies but can do very little for infants that become "stuck" and are unable to be delivered vaginally.
Lactation consultants assist the mother and newborn to emizish muvaffaqiyatli. A health visitor comes to see the mother and baby at home, usually within 24 hours of discharge, and checks the infant's adaptation to extrauterine life and the mother's postpartum physiological changes.
Non-western communities
Cultural values, assumptions, and practices of pregnancy and childbirth vary across cultures. Masalan, ba'zilari Mayya women who work in agricultural fields of some rural communities will usually continue to work in a similar function to how they normally would throughout pregnancy, in some cases working until labor begins.[159]
Yupatish and proximity to extended family and social support systems may be a childbirth priority of many communities in developing countries, such as the Chillihuani in Peru and the Mayan town of San Pedro La Laguna.[159][160] Home births can help women in these cultures feel more comfortable as they are in their own home with their family around them helping out in different ways.[159] Traditionally, it has been rare in these cultures for the mother to lie down during childbirth, opting instead for standing, kneeling, or walking around prior to and during birthing.[160][159]
Some communities rely heavily on religion for their birthing practices. It is believed that if certain acts are carried out, then it will allow the child for a healthier and happier future. One example of this is the belief in the Chillihuani that if a knife or scissors are used for cutting the kindik ichakchasi, it will cause for the child to go through clothes very quickly. In order to prevent this, a jagged ceramic tile is used to cut the umbilical cord.[160] In Mayan societies, ceremonial gifts are presented to the mother throughout pregnancy and childbirth in order to help her into the beginning of her child's life.[159]
Ceremonies and customs can vary greatly between countries. See;
Collecting stem cells
It is currently possible to collect two types of ildiz hujayralari during childbirth: amniotic stem cells and umbilical cord blood stem cells.[161] They are being studied as possible treatments of a number of conditions.[161]
Boshqa jihatlar
In many countries, age is reckoned from the date of birth, and sometimes the birthday is celebrated annually. Sharqiy Osiyo yoshini hisoblash starts newborns at "1", incrementing each Lunar Yangi yil.
Some cultures view the platsenta as a special part of birth, since it has been the child's life support for so many months. The placenta may be eaten by the newborn's family, ceremonially, for nutrition, or otherwise.[162] (Some animal mothers eat their afterbirth; this is called placentophagy.) Most recently there is a category of birth professionals available who will process the placenta for consumption by postpartum mothers.
Shuningdek qarang
- Tug'ruq paytida suiiste'mol qilish
- Ilg'or onalar yoshi, when a woman is of an older age at reproduction
- Antinatalism
- Asynclitic birth, an abnormal birth position
- Tug'ma nuqson
- Tug'ilish pozitsiyalari
- Tobut tug'ilishi
- Fergyuson refleksi
- Ko'p tug'ilish
- Obstetrical bleeding
- Naegele's rule, to calculate the due date for a pregnancy
- Natalizm
- Obstetrical Dilemma
- Perineal massage
- Pre- and perinatal psychology
- Reproductive Health Supplies Coalition
- An'anaviy tug'ilish xizmati
- Yordamsiz tug'ish
- Vernix caseosa
Natural birth topics:
Adabiyotlar
- ^ "confinement - Definition of confinement in English by Oxford Dictionaries". Oksford lug'atlari - ingliz tili.
- ^ "CONFINEMENT - meaning in the Cambridge English Dictionary". Kembrij lug'ati.
- ^ Lunze K, Bloom DE, Jamison DT, Hamer DH (January 2013). "The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival". BMC tibbiyoti. 11 (1): 24. doi:10.1186/1741-7015-11-24. PMC 3606398. PMID 23369256.
- ^ a b Martin RJ, Fanaroff AA, Walsh MC (2014-08-20). Fanaroff and Martin's Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. Elsevier sog'liqni saqlash fanlari. p. 116. ISBN 978-0-323-29537-6. Arxivlandi from the original on 2017-09-11.
- ^ a b v d e f Education material for teachers of midwifery : midwifery education modules (PDF) (2-nashr). Geneva [Switzerland]: World Health Organisation. 2008. p. 3. ISBN 978-92-4-154666-9. Arxivlandi (PDF) from the original on 2015-02-21.
- ^ a b Memon HU, Handa VL (May 2013). "Vaginal childbirth and pelvic floor disorders". Ayollar salomatligi. 9 (3): 265–77, quiz 276–77. doi:10.2217/whe.13.17. PMC 3877300. PMID 23638782.
- ^ a b Martin E (2015). Concise Colour Medical l.p.Dictionary. Oksford universiteti matbuoti. p. 375. ISBN 978-0-19-968799-2. Arxivlandi from the original on 2017-09-11.
- ^ a b "Dunyo faktlari kitobi". www.cia.gov. 2016 yil 11-iyul. Arxivlandi asl nusxasidan 2016 yil 16-noyabrda. Olingan 30 iyul 2016.
- ^ "Preterm birth Fact sheet N°363". JSSV. November 2015. Arxivlandi asl nusxasidan 2015 yil 7 martda. Olingan 30 iyul 2016.
- ^ Buck GM, Platt RW (2011). Reproductive and perinatal epidemiology. Oksford: Oksford universiteti matbuoti. p. 163. ISBN 978-0-19-985774-6. Arxivlandi from the original on 2017-09-11.
- ^ Co-Operation, Organisation for Economic; Development (2009). Doing better for children. Parij: OECD. p. 105. ISBN 978-92-64-05934-4. Arxivlandi from the original on 2017-09-11.
- ^ Olsen O, Clausen JA (September 2012). "Planned hospital birth versus planned home birth". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (9): CD000352. doi:10.1002/14651858.CD000352.pub2. PMC 4238062. PMID 22972043.
- ^ Fossard Ed, Bailey M (2016). Communication for Behavior Change: Volume lll: Using Entertainment–Education for Distance Education. SAGE nashrlari Hindiston. ISBN 978-93-5150-758-1. Arxivlandi from the original on 11 September 2017. Olingan 31 iyul 2016.
- ^ a b "Tug'ilish". The Columbia Electronic Encyclopedia (6 nashr). Kolumbiya universiteti matbuoti. 2016. Arxivlandi asl nusxasidan 2016-03-06. Olingan 2016-07-30 – via Encyclopedia.com.
- ^ a b v d e f g "Pregnancy Labor and Birth". Ayollar salomatligi. September 27, 2010. Arxivlandi from the original on 28 July 2016. Olingan 31 iyul 2016.
The first stage begins with the onset of labor and ends when the cervix is fully opened. It is the longest stage of labor, usually lasting about 12 to 19 hours
..
The second stage involves pushing and delivery of your baby. It usually lasts 20 minutes to two hours. - ^ McDonald SJ, Middleton P, Dowswell T, Morris PS (July 2013). "Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 7 (7): CD004074. doi:10.1002 / 14651858.CD004074.pub3. PMC 6544813. PMID 23843134.
- ^ a b Fillips, Raylin. "Tug'ilgandan so'ng darhol teridan teriga uzilishlar". Medscape. Arxivlandi asl nusxasidan 2015 yil 3 aprelda. Olingan 21 dekabr 2014.
- ^ a b "Antenatal, perinatal va tug'ruqdan keyingi parvarish" (PDF). Samarali perinatal yordamni targ'ib qilish. JSSV. Arxivlandi (PDF) asl nusxasidan 2015 yil 24 sentyabrda. Olingan 21 dekabr 2014.
- ^ a b "Tug'ruq paytida sog'lom ayollar va ularning chaqaloqlariga g'amxo'rlik qilish". Ayollar va bolalar salomatligini himoya qilish bo'yicha milliy hamkorlik markazi. Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti. Dekabr 2014. Arxivlangan asl nusxasi 2015 yil 12 fevralda. Olingan 21 dekabr 2014.
- ^ Hofmeyr GJ, Xanna M, Lawrie TA (iyul 2015). "Muddatni qisqa muddatda etkazib berish uchun rejalashtirilgan sezaryen". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (7): CD000166. doi:10.1002 / 14651858.CD000166.pub2. PMC 6505736. PMID 26196961.
- ^ "Tug'ilish va undan tashqarida". ayollar salomatligi.gov. 2016-12-13. Olingan 2018-11-20.
- ^ Tug'ilish: tug'ish, tug'ruq va tug'ruqdan keyingi tez yordam. Jahon Sog'liqni saqlash tashkiloti. 2015. p. D. bob. ISBN 978-92-4-154935-6. Arxivlandi asl nusxasidan 2017 yil 11 sentyabrda. Olingan 31 iyul 2016.
- ^ Molina G, Weiser TG, Lipsitz SR, Esquivel MM, Uribe-Leitz T, Azad T, Shoh N, Semrau K, Berry WR, Gawande AA, Xayns AB (dekabr 2015). "Sezaryen bilan tug'ilish darajasi va onalar va yangi tug'ilgan bolalar o'limi o'rtasidagi munosabatlar". JAMA. 314 (21): 2263–70. doi:10.1001 / jama.2015.15553. PMID 26624825.
- ^ a b Jahon Sog'liqni saqlash tashkiloti. "Yangi tug'ilgan chaqaloqlar: o'limni kamaytirish". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2017 yil 3 aprelda. Olingan 1 fevral 2017.
- ^ Weber SE (1996 yil yanvar). "Bola tug'adigan ayollarda og'riqning madaniy jihatlari". Akusherlik, ginekologik va neonatal hamshiralar jurnali. 25 (1): 67–72. doi:10.1111 / j.1552-6909.1996.tb02515.x. PMID 8627405.
- ^ Callister LC, Khalaf I, Semenic S, Kartchner R va boshq. (2003 yil dekabr). "Tug'ilish og'rig'i: madaniy xilma-xil ayollarning tasavvurlari". Og'riqni boshqarish bo'yicha hamshira. 4 (4): 145–54. doi:10.1016 / S1524-9042 (03) 00028-6. PMID 14663792.
- ^ Hodnett ED (may 2002). "Og'riq va ayollarning tug'ruq tajribasidan qoniqishi: muntazam ravishda qayta ko'rib chiqish". Amerika akusherlik va ginekologiya jurnali. 186 (5 Suppl tabiati): S160-72. doi:10.1016 / S0002-9378 (02) 70189-0. PMID 12011880.
- ^ Xarms, Rojert V. Orqa mehnat haqiqatan ham sodir bo'ladimi? Arxivlandi 2016-02-04 da Orqaga qaytish mashinasi, mayoclinic.com, Olingan 8 sentyabr 2014 yil
- ^ Meyer D (2007). "Selektiv serotoninni qaytarib olish inhibitörleri va ularning munosabatlarni qondirishga ta'siri". Oilaviy jurnal. 15 (4): 392–397. doi:10.1177/1066480707305470. S2CID 144945177.
- ^ Bowen R (2010 yil 12-iyul). "Oksitotsin". Biotibbiyot fanlari uchun gipermatnlar. Arxivlandi asl nusxasidan 2014 yil 29 avgustda. Olingan 2013-08-18.
- ^ Zlotnick C, Jonson SL, Miller IW, Pearlstein T va boshq. (2001 yil aprel). "Davlat yordamini olgan ayollarda tug'ruqdan keyingi depressiya: shaxslararo terapiya yo'naltirilgan guruh aralashuvini tajriba asosida o'rganish". Amerika psixiatriya jurnali. 158 (4): 638–40. doi:10.1176 / appi.ajp.158.4.638. PMID 11282702.
- ^ Chabrol H, Teissedre F, Saint-Jean M, Teisseyre N, Sistac C, Michaud C, Roge B (2002). "[Postpartum depressiyani aniqlash, oldini olish va davolash: 859 bemorni nazorat ostida o'rganish]". L'Encephale. 28 (1): 65–70. PMID 11963345.
- ^ Pillitteri A (2010). "15-bob: Mehnat va tug'ilish paytida oilaga hamshiralik yordami". Onalar va bolalar salomatligi bo'yicha hamshiralik: bolalarni parvarish qilish va bolalarni tarbiyalash oilasi. Xagerstaun, Merilend: Lippincott Uilyams va Uilkins. p. 350. ISBN 978-1-58255-999-5. Arxivlandi asl nusxasidan 2014-06-28. Olingan 2013-08-18.
- ^ Levine D (2012 yil 15 mart). "Yetkazib berishda ishlatiladigan forseps turlari". Sog'liqni saqlash tarmog'i. Sog'liqni saqlash tarmoqlari. Olingan 2013-08-10.
- ^ Goldberg AE (2018-03-02). "Serviksning pishishi". Medscape. Olingan 10 may, 2018.
- ^ Kupferminc M, Lessing JB, Yaron Y, Peyser MR (dekabr 1993). "Nifedipin va tug'ruqdan oldin tug'ruqni bostirish uchun ritodrin". Britaniya akusherlik va ginekologiya jurnali. 100 (12): 1090–94. doi:10.1111 / j.1471-0528.1993.tb15171.x. PMID 8297841. S2CID 24521943.
- ^ Jokic M, Guillois B, Cauquelin B, Giroux JD, Bessis JL, Morello R, Levy G, Balet JJ (mart 2000). "Xomilalik bezovtalik interlökin-6 va interleykin-8ni ko'paytiradi va infektsiyalanmagan to'liq tug'ilgan chaqaloqlarda o'sma nekrozi omil-alfa shnuri qon darajasini pasaytiradi". BJOG. 107 (3): 420–5. doi:10.1111 / j.1471-0528.2000.tb13241.x. PMID 10740342.
- ^ Lyrenäs S, Klon I, Ulmsten U (fevral, 2001). "In vivo jonli tug'ruq paytida vaginal qo'shimchadan (0,8 mm, 10 mg) PGE2 ning boshqarilishi". BJOG. 108 (2): 169–78. doi:10.1111 / j.1471-0528.2001.00039.x. PMID 11236117. S2CID 45247771.
- ^ Giacalone PL, Vignal J, Daures JP, Boulot P, Hedon B, Laffargue F (mart 2000). "Postpartum qon ketish xavfi past bo'lgan ayollarda tug'ruqning uchinchi bosqichini boshqarishning ikkita texnikasini tasodifiy baholash". BJOG. 107 (3): 396–400. doi:10.1111 / j.1471-0528.2000.tb13236.x. PMID 10740337.
- ^ Xantoushzadeh S, Alhusseini N, Lebaschi AH (2007 yil fevral). "Tug'ruq paytida akupunkturaning nullipar ayollarga ta'siri: tasodifiy nazorat ostida sinov". Avstraliya va Yangi Zelandiya akusherlik va ginekologiya jurnali. 47 (1): 26–30. doi:10.1111 / j.1479-828X.2006.00674.x. PMID 17261096. S2CID 23495692.
- ^ a b v d "Mehnat va tug'ruq, tug'ruqdan keyingi parvarish". Mayo klinikasi. Olingan 7 may, 2018.
- ^ Novak S. "Chaqaloqlar tug'ilishining eng mashhur vaqti". Vashington Post. Arxivlandi asl nusxasi 2018-06-16. Olingan 2018-05-09.
- ^ Reiter RJ, Tan DX, Korkmaz A, Rosales-Corral SA (2013). "Melatonin va barqaror tsirkadiyalik ritmlar ona, platsenta va homila fiziologiyasini optimallashtiradi". Inson ko'payishining yangilanishi. 20 (2): 293–307. doi:10.1093 / humupd / dmt054. PMID 24132226.
- ^ Saten AJ (2013 yil 1-iyul). "Mehnatning yashirin bosqichi". Hozirgi kungacha. Wolters Kluwer. Arxivlandi asl nusxasidan 2016 yil 3 martda.(obuna kerak)
- ^ Murray LJ, Hennen L, Scott J (2005). BabyCenter homiladorlik va tug'ish bo'yicha muhim qo'llanma: eng yaxshi homiladorlik va ota-ona uchun mutaxassislarning maslahati va haqiqiy donoligi. Emmaus, Pensilvaniya: Rodale kitoblari. pp.294 –295. ISBN 978-1-59486-211-3. Olingan 2013-08-18.
- ^ Mayo klinikasi xodimlari. "Servikal bo'shliq va kengayish". Mayo klinikasi. Arxivlandi asl nusxasidan 2016 yil 4 dekabrda. Olingan 31 yanvar 2017.
- ^ "JSST tomonidan tug'ruqdan keyingi ijobiy parvarish tajribasi uchun tug'ruqdan oldin parvarish qilish bo'yicha tavsiyalar (Tavsiya 5)" (PDF). Jahon Sog'liqni saqlash tashkiloti. Olingan 6 may, 2018.
- ^ Akusherlik ma'lumotlarini aniqlash masalalari va o'zgarishlarning asoslari Arxivlandi 2013-11-06 da Orqaga qaytish mashinasi, 2012 yil ACOG.
- ^ Boyl A, Reddy UM, Landy HJ, Huang CC, Driggers RW, Laughon SK (iyul 2013). "Qo'shma Shtatlarda birlamchi sezaryen bilan tug'ilish". Akusherlik va ginekologiya. 122 (1): 33–40. doi:10.1097 / AOG.0b013e3182952242. PMC 3713634. PMID 23743454.
- ^ "JSST tug'ruqdan keyingi parvarishlash bo'yicha ijobiy tug'ruq tajribasini tavsiya qiladi (3.2.2-band)." (PDF). Jahon Sog'liqni saqlash tashkiloti. Olingan 6 may, 2018.
- ^ Zhang J, Troendle JF, Yancey MK (oktyabr 2002). "Nullipar ayollarda mehnat egri chizig'ini qayta baholash". Amerika akusherlik va ginekologiya jurnali. 187 (4): 824–28. doi:10.1067 / mob.2002.127142. PMID 12388957. Arxivlandi asl nusxasidan 2016-01-18.
- ^ "Anormal mehnat". Medscape. Olingan 14 may, 2018.
- ^ "JSST tomonidan tug'ruqdan keyingi parvarish qilish bo'yicha ijobiy tug'ruq tajribasi (№ 33 band)" (PDF). Jahon Sog'liqni saqlash tashkiloti. Olingan 6 may, 2018.
- ^ Rouse DJ, Weiner SJ, Bloom SL, Varner MW va boshq. (Oktyabr 2009). "Nullipar ayollarda tug'ruqning ikkinchi bosqichi: onalik va perinatal natijalar bilan bog'liqlik". Amerika akusherlik va ginekologiya jurnali. 201 (4): 357.e1-7. doi:10.1016 / j.ajog.2009.08.003. PMC 2768280. PMID 19788967.
- ^ Jangsten E, Mattsson LÅ, Lyckestam I, Hellström AL va boshq. (2011 yil fevral). "Mehnatning uchinchi bosqichini faol boshqarish va kutilayotgan boshqaruvni taqqoslash: shved randomizatsiyalangan nazorat ostida sinov". BJOG. 118 (3): 362–69. doi:10.1111 / j.1471-0528.2010.02800.x. PMID 21134105.
- ^ Milodiy haftalar (2008 yil dekabr). "Saqlanib qolgan platsenta". Eng yaxshi amaliyot va tadqiqot. Klinik akusherlik va ginekologiya. 22 (6): 1103–17. doi:10.1016 / j.bpobgyn.2008.07.005. PMID 18793876.
- ^ To'p H (iyun 2009). "Ba'zi bir rivojlanayotgan mamlakatlarda uchinchi mehnat holatini faol boshqarish kamdan-kam uchraydi". Jinsiy va reproduktiv salomatlikning xalqaro istiqbollari. 35 (2). Arxivlandi asl nusxasidan 2016-03-04.
- ^ Stanton C, Armbruster D, Knight R, Ariawan I va boshq. (Mart 2009). "Yettita rivojlanayotgan mamlakatda mehnatning uchinchi bosqichini faol boshqarish usullaridan foydalanish". Jahon sog'liqni saqlash tashkilotining Axborotnomasi. 87 (3): 207–15. doi:10.2471 / BLT.08.052597. PMC 2654655. PMID 19377717.
- ^ Xalqaro doyalar konfederatsiyasi; Xalqaro ginekologlar akusherlik federatsiyasi (2004). "Qo'shma bayonot: tug'ruqdan keyingi qon ketishining oldini olish uchun tug'ruqning uchinchi bosqichini boshqarish". Akusherlik va ayollar salomatligi jurnali. 49 (1): 76–77. doi:10.1016 / j.jmwh.2003.11.005. PMID 14710151.
- ^ Mathai M, Gulmezoglu AM, Hill S (2007). "VOZning tug'ruqdan keyingi qon ketishining oldini olish bo'yicha tavsiyalari" (PDF). Jeneva: Jahon Sog'liqni saqlash tashkiloti, Homiladorlikni xavfsizroq qilish bo'limi. Arxivlandi asl nusxasi (PDF) 2009-07-05 da. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ McDonald SJ, Middleton P, Dowswell T, Morris PS (iyul 2013). McDonald SJ (tahrir). "Tug'ilgan chaqaloqlarni kindik ichakchasidagi qisish vaqtining onalik va neonatal natijalariga ta'siri". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 7 (7): CD004074. doi:10.1002 / 14651858.CD004074.pub3. PMC 6544813. PMID 23843134.
- ^ Kempbell D (2013-07-10). "Kasalxonalar tug'ilgandan keyin kindik ichaklarini kesishni kechiktirish kerakligi to'g'risida ogohlantirildi". The Guardian. Olingan 11 iyun, 2018.
- ^ Gjerdingen DK, Froberg DG (1991 yil yanvar). "Mehnatning to'rtinchi bosqichi: tug'ruqdan keyingi olti haftalikdagi tug'ma onalar va farzand asrab oluvchilarning salomatligi". Oilaviy tibbiyot. 23 (1): 29–35. PMID 2001778.
- ^ a b JSST (2013). "JSST onaga va yangi tug'ilgan chaqaloqqa tug'ruqdan keyingi parvarish bo'yicha tavsiyalar". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2014 yil 22 dekabrda. Olingan 22 dekabr 2014.
- ^ Whitaker, Amy K.; Chen, Beatrice A. (2017 yil 5-oktabr). "Oila rejalashtirish bo'yicha ko'rsatmalar jamiyati: intrauterin vositalarni platsentadan keyingi kiritish". Kontratseptsiya (2018 yil yanvarda nashr etilgan). 97 (1): 2–13. doi:10.1016 / j.contraception.2017.09.014. ISSN 0010-7824. PMID 28987293.
- ^ "Tug'ilgandan so'ng darhol uzoq muddatli ta'sir ko'rsatadigan kontratseptsiya". www.acog.org. Olingan 2020-04-20.
- ^ "Tug'ruqdan keyingi baholash". ATI hamshiralik ta'limi. Arxivlandi asl nusxasi 2014 yil 24 dekabrda. Olingan 24 dekabr 2014.
- ^ Mayo klinikasi xodimlari. "Tug'ruqdan keyingi parvarish: qinidan keyin nima kutish mumkin". Mayo klinikasi. Arxivlandi asl nusxasidan 2014 yil 21 dekabrda. Olingan 23 dekabr 2014.
- ^ Saloojee H (2008 yil 4-yanvar). "Onalar va ularning sog'lom tug'ilgan chaqaloqlari uchun teridan teriga erta murojaat qilish". JSST Reproduktiv salomatlik kutubxonasi. JSSV. Arxivlandi asl nusxasidan 2014 yil 21 dekabrda. Olingan 23 dekabr 2014.
- ^ Crenshaw J (2007). "6-sonli parvarish amaliyoti: ona va bolani ajratmaslik, emizish uchun cheksiz imkoniyatlar bilan". Perinatal ta'lim jurnali. 16 (3): 39–43. doi:10.1624 / 105812407X217147. PMC 1948089. PMID 18566647.
- ^ Mur ER, Bergman N, Anderson GC, Medley N (noyabr 2016). "Onalar va ularning sog'lom tug'ilgan chaqaloqlari uchun teridan teriga erta murojaat qilish". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 11: CD003519. doi:10.1002 / 14651858.CD003519.pub4. PMC 3979156. PMID 27885658.
- ^ Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, King VJ, Keeton KL (oktyabr 2011). "Mehnatni induktsiya qilish usullari: tizimli ko'rib chiqish". BMC Homiladorlik va tug'ish. 11: 84. doi:10.1186/1471-2393-11-84. PMC 3224350. PMID 22032440.
- ^ a b "Umumiy sezaryen, birlamchi sezaryen va sezaryen so'ng qin bilan tug'ilish stavkalari (VBAC), Amerika Qo'shma Shtatlari, 1989-2010" (PDF). Tug'ruqqa ulanish veb-sayt. Sezaryen kursining tinimsiz ko'tarilishi. Avgust 2012. Arxivlangan asl nusxasi (PDF) 2013-02-17. Olingan 2013-08-29.
- ^ Asosiy E, Oshiro B, Chagolla B, Bingem D, Dang-Kilduff L, Kovalevskiy L (2010 yil iyul). "39 haftalik homiladorlik davridan oldin tibbiy ko'rsatilmagan (tanlov asosida) etkazib berishni bekor qilish (onalikni parvarish qilishni o'zgartirish uchun Kaliforniyadagi onalarga sifatli tibbiy yordam ko'rsatish bo'yicha qo'llanma)" (PDF). Bilan 08.05012-sonli shartnoma asosida ishlab chiqilgan Kaliforniya sog'liqni saqlash boshqarmasi; Onalar, bolalar va o'spirinlar salomatligi bo'limi. (1-nashr). Dimes marti. Arxivlandi asl nusxasi (PDF) 2012-11-20. Olingan 2013-08-29. Iqtibos jurnali talab qiladi
| jurnal =(Yordam bering) - ^ "Homiladorlik davri bo'yicha ish haqining so'nggi pasayishi". Kasalliklarni nazorat qilish va oldini olish markazlari. Olingan 9-may, 2018.
- ^ Martin JA, Xemilton BE, Satton PD, Ventura SJ, Mathews TJ, Kirmeyer S, Osterman MJ (avgust 2010). "Tug'ilishlar: 2007 yildagi yakuniy ma'lumotlar" (PDF). Milliy hayotiy statistik hisobotlar: Kasalliklarni nazorat qilish va oldini olish markazlaridan, Sog'liqni saqlash bo'yicha milliy statistika markazi, Milliy hayotiy statistika tizimi. 58 (24): 1–85. PMID 21254725. Arxivlandi (PDF) asl nusxasidan 2013 yil 21 avgustda.
- ^ ACOG tuman II kasal xavfsizligi va sifatini yaxshilash qo'mitasi (2011 yil dekabr). "Induksiya uchun oksitotsin" (PDF). Akusherlikdagi protokollarni optimallashtirish. 1-seriya. Amerika akusher-ginekologlar Kongressi (ACOG). Arxivlandi asl nusxasi (PDF) 2013-06-21. Olingan 2013-08-29.
- ^ "Sog'liqni saqlashning malakali xodimlari ishtirok etgan tug'ilish ulushi". Ma'lumotlardagi bizning dunyomiz. Olingan 5 mart 2020.
- ^ Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti. "Bachadon ichi parvarish: tug'ruq paytida sog'lom ayollar va ularning chaqaloqlariga g'amxo'rlik qilish". Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti. Arxivlandi asl nusxasidan 2015 yil 18 fevralda. Olingan 11 fevral 2015.
- ^ Tranmer JE, Xodnett ED, Xanna ME, Stivens BJ (2005). "Cheklovsiz karbongidrat iste'mol qilishning mehnat o'sishiga ta'siri". Akusherlik, ginekologik va neonatal hamshiralar jurnali. 34 (3): 319–28. doi:10.1177/0884217505276155. PMID 15890830.
- ^ O'Sullivan G, Scrutton M (2003 yil mart). "Tug'ruq paytida NPO. Ilmiy tekshirish bormi?". Shimoliy Amerikaning behushlik klinikalari. 21 (1): 87–98. doi:10.1016 / S0889-8537 (02) 00029-9. PMID 12698834.
- ^ Singata M, Tranmer J, Gyte GM (avgust 2013). Singata M (tahrir). Homiladorlik va tug'ish guruhi. "Tug'ruq paytida og'iz orqali suyuqlik va ovqat iste'mol qilishni cheklash". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 8 (8): CD003930. doi:10.1002 / 14651858.CD003930.pub3. PMC 4175539. PMID 23966209. Xulosa – Cochrane xulosalari (2013-08-22).
- ^ Basevi V, Lavender T (2014 yil noyabr). "Ishga qabul qilishda muntazam ravishda perineal sochingizni". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (11): CD001236. doi:10.1002 / 14651858.CD001236.pub2. PMC 7076285. PMID 25398160.
- ^ Lumbiganon P, Thinkhamrop J, Thinkhamrop B, Tolosa JE (sentyabr 2014). "Onalik va neonatal infektsiyalarni oldini olish uchun tug'ruq paytida vaginal xlorhexidin (B guruhi Streptokokk va OIV bundan mustasno)". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 9 (9): CD004070. doi:10.1002 / 14651858.CD004070.pub3. PMC 7104295. PMID 25218725.
- ^ Xas, Devid M.; Morgan, Sara; Contreras, Karenrose; Kimball, Savannah (2020 yil 26-aprel). "Operatsiyadan keyingi infektsiyalarni oldini olish uchun sezaryen oldin antiseptik eritma bilan vaginal preparat". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 4: CD007892. doi:10.1002 / 14651858.CD007892.pub7. ISSN 1469-493X. PMC 7195184. PMID 32335895.
- ^ "Forseps yoki vakuum bilan etkazib berish". NHS. Olingan 15-noyabr, 2020.
- ^ Jons L, Usmon M, Dovsvel T, Alfirevich Z, Geyts S, Newburn M, Jordan S, Lavender T, Neilson JP (mart 2012). "Mehnatga chalingan ayollar uchun og'riqni boshqarish: muntazam tekshiruvlarga umumiy nuqtai". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 3 (3): CD009234. doi:10.1002 / 14651858.CD009234.pub2. PMC 7132546. PMID 22419342.
- ^ Amerika Pediatriya Akademiyasining yangi tug'ilgan chaqaloq homilasi bo'yicha qo'mitasi; Amerikalik akusherlik kolleji ginekologlari akusherlik amaliyoti bo'yicha qo'mitasi (2014 yil aprel). "Tug'ruq paytida va tug'ruq paytida suvga cho'mish". Pediatriya. 133 (4): 758–61. doi:10.1542 / peds.2013-3794. PMID 24652300.
- ^ Bohren MA, Xofmeyr GJ, Sakala S, Fukuzava RK, Kutbert A (iyul 2017). "Tug'ruq paytida ayollarni doimiy qo'llab-quvvatlash". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 7: CD003766. doi:10.1002 / 14651858.CD003766.pub6. PMC 6483123. PMID 28681500.
- ^ Caughey AB, Cahill AG, Guise JM, Rouse DJ (mart 2014). "Birlamchi sezaryen bilan tug'ilishning xavfsiz oldini olish". Amerika akusherlik va ginekologiya jurnali. 210 (3): 179–93. doi:10.1016 / j.ajog.2014.01.026. PMID 24565430.
- ^ Lancashire, Liz (2018 yil 9-iyul). "Ebalar uchun tibbiyot ma'muriyati". Norfolk va Norvich universiteti kasalxonalari. Olingan 16 iyun, 2019.
- ^ Thorp JA, Breedlove G (iyun 1996). "Tug'ilishda epidural analjeziya: xatar va foydalarni baholash". Tug'ilish. 23 (2): 63–83. doi:10.1111 / j.1523-536X.1996.tb00833.x. PMID 8826170.
- ^ a b Anim-Somuah M, Smit RM, Cyna AM, Kutbert A (may 2018). "Epidural va epidural bo'lmagan yoki og'riqsizlantirish paytida og'riqni boshqarish uchun og'riqsizlantirish". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 5: CD000331. doi:10.1002 / 14651858.CD000331.pub4. PMC 6494646. PMID 29781504.
- ^ Alehagen S, Vijma B, Lundberg U, Vijma K (sentyabr 2005). "Tug'ruq paytida qo'rquv, og'riq va stress gormonlari". Psixosomatik akusherlik va ginekologiya jurnali. 26 (3): 153–65. doi:10.1080/01443610400023072. PMID 16295513. S2CID 44646591.
- ^ Loftus JR, Hill H, Koen SE (avgust 1995). "Tug'ruq paytida bupivakain bilan yuborilgan epidural sufentanil va fentanilning platsenta o'tkazilishi va neonatal ta'siri". Anesteziologiya. 83 (2): 300–308. doi:10.1097/00000542-199508000-00010. PMID 7631952.
- ^ Vey SQ, Luo ZC, Xu H, Freyzer VD (sentyabr 2009). "Erta oksitotsinni ko'paytirishning tug'ruqdagi ta'siri: meta-tahlil". Akusherlik va ginekologiya. 114 (3): 641–49. doi:10.1097 / AOG.0b013e3181b11cb8. PMID 19701046. S2CID 29571476.
- ^ "Mehnatni ko'paytirish bo'yicha tavsiyalar" (PDF). Jahon Sog'liqni saqlash tashkiloti. Olingan 9-may, 2018.
- ^ Jiang H, Qian X, Carroli G, Garner P (2017 yil fevral). "Qin bilan tug'ilish uchun epizyotomiyani selektiv va muntazam ravishda qo'llash". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 2: CD000081. doi:10.1002 / 14651858.CD000081.pub3. PMC 5449575. PMID 28176333.
- ^ Bastos, Mariya Xelena; Furuta, Mari; Kichik, Rhonda; McKenzie-McHarg, Kirstie; Bick, Debra (2015-04-10). "Tug'ilgandan keyingi ayollarda psixologik travmanın oldini olish bo'yicha xulosalar". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (4): CD007194. doi:10.1002 / 14651858.CD007194.pub2. ISSN 1469-493X. PMID 25858181.
- ^ Vernon D (2007 yil 6-fevral). "Tug'ilganda erkaklar - sizning blokiniz u erda bo'lishi kerakmi?". BellyBelly.com.au. Arxivlandi asl nusxasidan 2013-06-01. Olingan 2013-08-23.
- ^ Boren, MA; Xofmeyr, GJ; Sakala, C; Fukuzava, RK; Kutbert, A (6-iyul, 2017-yil). "Tug'ruq paytida ayollarni doimiy qo'llab-quvvatlash". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 7: CD003766. doi:10.1002 / 14651858.CD003766.pub6. PMC 6483123. PMID 28681500.
- ^ Xammond P, Jonson A (1986). "Tokodinamometr". Jigarrang M (tahrir). Tibbiy asboblar lug'ati. London: Chapman va Xoll. ISBN 978-0-412-28290-4. Arxivlandi asl nusxasidan 2016-03-04. Olingan 2013-08-23. Onlayn versiyaga kirildi.
- ^ Alfirevich, Zarko; Gayt, Gillian ML; Kutbert, Anna; Devane, Deklan (2017). "Uzluksiz kardiotokografiya (CTG) homila tug'ruq paytida uni baholash uchun elektron homila monitoringi (EFM) shakli sifatida". Tizimli sharhlarning Cochrane ma'lumotlar bazasi. 2: CD006066. doi:10.1002 / 14651858.CD006066.pub3. PMC 6464257. PMID 28157275. Olingan 6 may, 2018.
- ^ "JSST tug'ruqdan keyingi parvarish bo'yicha ijobiy tug'ruq tajribasini tavsiya qiladi (17-TAVSIYA)" (PDF). Jahon Sog'liqni saqlash tashkiloti. Olingan 7 may, 2018.
- ^ a b "JSSTga a'zo davlatlar uchun o'lim va kasallik og'irligini baholash 2004 yilda" (xls). Jahon sog'liqni saqlash tashkiloti o'lchov va sog'liqni saqlash bo'yicha ma'lumotlar bo'limi. Arxivlandi asl nusxasidan 2014-02-02.
- ^ "Onalar salomatligi". Birlashgan Millatlar Tashkilotining Aholi jamg'armasi. Olingan 24 aprel, 2018.
- ^ Van Lerberghe V, De Brouere V (2001). "Ko'zi ojizlar va ishlagan narsalar to'g'risida: Onalar o'limini kamaytirish bo'yicha tarix darslari" (PDF). De Brouere V, Van Lerberghe V (tahr.). Xavfsiz onalik strategiyasi: dalillarni qayta ko'rib chiqish. Sog'liqni saqlash xizmatlarini tashkil etish va siyosat bo'yicha tadqiqotlar. 17. Antverpen: ITG Press. 7-33 betlar. ISBN 978-90-76070-19-3.
Onalik o'limini oldini olish uchun hech qanday samarali choralar ko'rilmagan joyda, "tabiiy" o'lim, ehtimol 1500/100000 darajaga teng.
- ^ "AQSh rivojlangan dunyoda onalar o'limining eng yomon ko'rsatkichiga ega". Milliy radio. Olingan 25 aprel, 2018.
- ^ "Tug'ruq paytida ayollarning og'ir asoratlari osmonga ko'tarilmoqda - ko'pincha oldini olish mumkin". ProPublica. 2017-12-22. Olingan 4-may, 2018.
- ^ Levi J, Kon D, Jonson K (iyun 2011). "Sog'lom ayollar, sog'lom bolalar: sog'liqni saqlash sohasidagi islohotlar Amerikadagi ayollar va chaqaloqlarning sog'lig'ini qanday yaxshilaydi" (PDF). Vashington, Kolumbiya: Amerika sog'lig'iga ishonish. Arxivlandi (PDF) asl nusxasidan 2012-06-24. Olingan 2013-08-29.
- ^ Akusherlik o'qituvchilari uchun o'quv materiali: akusherlik ta'lim modullari (PDF) (2-nashr). Jeneva [Shveytsariya]: Jahon sog'liqni saqlash tashkiloti. 2008. 38-44 betlar. ISBN 9789241546669. Arxivlandi (PDF) asl nusxasidan 2015-02-21.
- ^ Glazener CM, Abdalla M, Stroud P, Naji S, Templeton A, Rassell IT (aprel 1995). "Postnatal onalik kasalligi: darajasi, sabablari, oldini olish va davolash". Britaniya akusherlik va ginekologiya jurnali. 102 (4): 282–87. doi:10.1111 / j.1471-0528.1995.tb09132.x. PMID 7612509. S2CID 38872754.
- ^ Tompson JF, Roberts CL, Currie M, Ellwood DA (iyun 2002). "Tug'ilgandan keyin sog'liq muammolarining tarqalishi va davom etishi: tug'ilishning tengligi va uslubiga bog'liqlik". Tug'ilish. 29 (2): 83–94. doi:10.1046 / j.1523-536X.2002.00167.x. PMID 12051189.
- ^ Chegaralar N (2006). "Tug'ilgandan so'ng: tug'ruqdan keyingi sog'lig'ini tug'ruq uslubiga nisbatan tanqidiy ko'rib chiqish". Akusherlik va ayollar salomatligi jurnali. 51 (4): 242–248. doi:10.1016 / j.jmwh.2005.10.014. PMID 16814217.
- ^ Jaju S, Al Kharusi L, Gowri V (2015). "Primigravid ayollarida tug'ruq va tushkun kayfiyat bilan bog'liq qo'rquvning antenatal tarqalishi". Hindiston psixiatriya jurnali. 57 (2): 158–61. doi:10.4103/0019-5545.158152. PMC 4462784. PMID 26124521.
- ^ Lukasse M, Schei B, Ryding EL (oktyabr 2014). "Evropaning oltita mamlakatida tug'ilish qo'rquvining tarqalishi va shu bilan bog'liq omillar". Jinsiy va reproduktiv sog'liqni saqlash. 5 (3): 99–106. doi:10.1016 / j.srhc.2014.06.007. hdl:10642/2246. PMID 25200969.
- ^ a b "Tug'ilgandan keyingi depressiya faktlari". Milliy ruhiy salomatlik instituti. Olingan 4-may, 2018.
- ^ Lapp LK, Agbokou C, Peretti CS, Ferreri F (sentyabr 2010). "Tug'ilgandan keyingi travmatik stressni boshqarish: qayta ko'rib chiqish". Psixosomatik akusherlik va ginekologiya jurnali. 31 (3): 113–22. doi:10.3109 / 0167482X.2010.503330. PMID 20653342. S2CID 23594561.
- ^ Condon J (2010 yil fevral). "Ayollarning ruhiy salomatligi: DSM V uchun" istaklar ro'yxati "". Ayollarning ruhiy salomatligi arxivi. 13 (1): 5–10. doi:10.1007 / s00737-009-0114-1. PMID 20127444. S2CID 1102994.
- ^ Martin S (2012). Perinatal ruhiy salomatlik: Klinik qo'llanma. Cumbria Angliya: M & K Pub. p. 26. ISBN 9781907830495.
- ^ Alder J, Stadlmayr V, Tschudin S, Bitzer J (iyun 2006). "Tug'ilgandan keyingi travmatik alomatlar: biz nimani taklif qilishimiz kerak?". Psixosomatik akusherlik va ginekologiya jurnali. 27 (2): 107–12. doi:10.1080/01674820600714632. PMID 16808085. S2CID 21859634.
- ^ a b Jons I, Chandra PS, Dazzan P, Xovard LM (2014 yil noyabr). "Homiladorlik va tug'ruqdan keyingi davrda bipolyar buzilish, affektiv psixoz va shizofreniya". Lanset. 384 (9956): 1789–99. doi:10.1016 / S0140-6736 (14) 61278-2. PMID 25455249. S2CID 44481055.
- ^ "Tug'ilish: umumiy nuqtai". NICHD. 23 sentyabr 2014 yil. Arxivlandi asl nusxasidan 2016 yil 5 oktyabrda. Olingan 4 oktyabr 2016.
- ^ a b v d e f "Tug'ilganlar". Jahon Sog'liqni saqlash tashkiloti. Arxivlandi asl nusxasidan 2016-10-02. Olingan 2016-09-29.
- ^ "O'lik tug'ilishning oldini olish mumkin. Lanset seriyasining qisqacha mazmuni" (PDF). Lanset. Yanvar 2016. Arxivlangan asl nusxasi (PDF) 2018-07-12. Olingan 2020-01-31.
- ^ "Tibbiy xodimlar o'lik tug'ilishni qanday boshqaradi?". NICHD. 23 sentyabr 2014 yil. Arxivlandi asl nusxasidan 2016 yil 5 oktyabrda. Olingan 4 oktyabr 2016.
- ^ "Tug'ilish: boshqa savollar". NICHD. 23 sentyabr 2014 yil. Arxivlandi asl nusxasidan 2016 yil 5 oktyabrda. Olingan 4 oktyabr 2016.
- ^ a b "O'lik tug'ilish qanchalik keng tarqalgan?". NICHD. 23 sentyabr 2014 yil. Arxivlandi asl nusxasidan 2016 yil 5 oktyabrda. Olingan 4 oktyabr 2016.
- ^ Draper, Elizabeth S.; Manktelov, Bredli N.; Smit, Lyusi; Rubayet, Sayed; Xirst, Jeyn; Neyman, Melissa; Qirol, Karina; Osrin, Devid; Prost, Audrey (2016-02-06). "O'lik tug'ilish: stavkalar, xavf omillari va 2030 yilgacha tezlashish". Lanset. 387 (10018): 587–603. doi:10.1016 / S0140-6736 (15) 00837-5. ISSN 0140-6736. PMID 26794078.
- ^ "Erta tug'ilish". Jahon Sog'liqni saqlash tashkiloti. Olingan 26 aprel, 2018.
- ^ "JSSTga a'zo davlatlar uchun o'lim va kasallik og'irligini baholash 2004 yilda" (xls). Jahon sog'liqni saqlash tashkiloti o'lchov va sog'liqni saqlash bo'yicha ma'lumotlar bo'limi. 2009 yil fevral.
- ^ Ohlsson A, Shoh VS (iyun 2014). "Ma'lum bo'lgan ona guruhi B streptokokk kolonizatsiyasi uchun tug'ruq ichidagi antibiotiklar". Tizimli sharhlarning Cochrane ma'lumotlar bazasi (6): CD007467. doi:10.1002 / 14651858.CD007467.pub4. PMID 24915629.
- ^ "Jinsiy yo'l bilan yuqadigan yuqumli kasalliklar (STI)". Jahon Sog'liqni saqlash tashkiloti. 2013 yil may. Arxivlandi asl nusxasidan 2014-11-25. Olingan 2013-08-30.
- ^ van Xandel M, Swaab H, de Vriz LS, Jongmans MJ (2007 yil iyul). "Perinatal asfiksiyadan so'ng neonatal ensefalopatiyaning uzoq muddatli kognitiv va xulq-atvori oqibatlari: ko'rib chiqish". Evropa pediatriya jurnali. 166 (7): 645–54. doi:10.1007 / s00431-007-0437-8. PMC 1914268. PMID 17426984.
- ^ Uorvik R, Uilyams PL, nashr. (1973). Greyning anatomiyasi (35-ingliz nashri). London: Longman. p. 1046. ISBN 978-0-443-01011-8.
- ^ a b v d e f g h men Xutter Epshteyn, MD, Randi (2011). Meni chiqaring: Adan bog'idan Spermatozoidlargacha bo'lgan tug'ilish tarixi. Nyu-York: W.W. Norton & Company, Inc.
- ^ a b Bo'yoq NS (1980 yil kuz). "Amerikada tug'ilish tarixi". Ayollar: Jinsiy aloqa va shahvoniylik, 2-qism. Chikago universiteti matbuoti. 6 (1): 97–108. doi:10.1086/493779. JSTOR 3173968. PMID 21213655.
- ^ Leavitt, Judith W. (1988). Yotoqqa olib kelingan: Amerikada bolani tug'ish, 1750-1950. Oksford universiteti. 90-91 betlar. ISBN 978-0-19-505690-7.
- ^ "Otalar va teridan teriga aloqa". Kenguru ona parvarishi. Olingan 30 aprel 2013.
- ^ Kessidi T (2006). Tug'ilish. Nyu-York: Atlantic Monthly Press. pp.54–55. ISBN 978-0-87113-938-2.
- ^ a b v Loudon I (2000 yil iyul). "O'tmishda onalar o'limi va uning rivojlanayotgan mamlakatlar uchun dolzarbligi". Amerika Klinik Ovqatlanish Jurnali. 72 (1 ta qo'shimcha): 241S-246S. doi:10.1093 / ajcn / 72.1.241S. PMID 10871589.
- ^ a b Tompson CJ (2005). "Refleksiv shubha uyushmasida iste'molchilarning xatarlarini qabul qilish". Iste'molchilarni tadqiq qilish jurnali. 32 (2): 235–248. doi:10.1086/432233.
- ^ a b Tabiiy jarayonmi? Ayollar, erkaklar va tug'ruqni tibbiylashtirish ". olib keldi.tizim.sciencemuseum.org.uk. Qabul qilingan 2018-12-03.
- ^ a b Rosenthal E (2013-06-30). "Dunyoda eng qimmat bo'lgan Amerikaning tug'ilish usuli - NYTimes.com". The New York Times. Arxivlandi asl nusxasidan 2017-01-01.
- ^ Barrett ML, Smit MW, Elizhauzer A, Honigman LS, Pines JM (dekabr 2014). "Reanimatsiya xizmatidan foydalanish, 2011 yil". HCUP Statistik qisqacha ma'lumot # 185. Rokvill, MD: Sog'liqni saqlash tadqiqotlari va sifat agentligi. Arxivlandi asl nusxasidan 2015-04-02.
- ^ Hsia RY, Akosa Antwi Y, Weber E (yanvar 2014). "Vaginal va sezaryen bilan tug'ilish uchun to'lovlar va narxlar o'zgarishini tahlil qilish: tasavvurlarni o'rganish". BMJ ochiq. 4 (1): e004017. doi:10.1136 / bmjopen-2013-004017. PMC 3902513. PMID 24435892.

- ^ Ayollar va bolalar salomatligini himoya qilish bo'yicha milliy hamkorlik markazi (2007). Bachadon ichi parvarish: tug'ruq paytida sog'lom ayollar va ularning bolalariga g'amxo'rlik qilish. NICE Klinik qo'llanmasi, № 55. London: RCOG. PMID 21250397.[sahifa kerak ]
- ^ "Tavsiyalar: sog'lom ayollar va chaqaloqlarga tug'ruqdan oldin parvarish qilish". Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti. Sog'liqni saqlash va g'amxo'rlikning mukammalligi milliy instituti. Olingan 6 dekabr 2020.
- ^ Bennold K, Lui KS (2014-12-03). "Britaniyalik regulyator asoratlanmagan homiladorlik uchun kasalxonalar orqali uy sharoitida tug'ilishni talab qilmoqda - NYTimes.com". The New York Times. Arxivlandi asl nusxasidan 2017-03-28.
- ^ Stearns PN, ed. (1993-12-21). Ijtimoiy tarix ensiklopediyasi. Ijtimoiy fanlarning Garland ma'lumotnomasi. V. 780. London: Teylor va Frensis. p. 144. ISBN 978-0-8153-0342-8. Arxivlandi asl nusxasidan 2016-01-02.
- ^ a b v Tait HN, Cidro J (fevral, 2018). Homiladorlik va tug'ilishning mahalliy tajribalari. ISBN 9781772581355. OCLC 1012401274.
- ^ "Qamoqdagi enaga nima". NannySOS. Arxivlandi asl nusxasidan 2016 yil 20 dekabrda. Olingan 22 dekabr 2016.
- ^ "AMCB to'g'risida". Arxivlandi asl nusxasidan 2014-02-23. Olingan 2014-02-20.
- ^ "Britaniya Kolumbiyasi doyalar kollejiga xush kelibsiz". Britaniya Kolumbiyasi doyalar kolleji veb-sayti. Arxivlandi asl nusxasidan 2013-09-17. Olingan 2013-08-30.
- ^ Britaniya Kolumbiyasi viloyati (2013 yil 21 avgust) [Britaniya Kolumbiyasining qayta ko'rib chiqilgan haykallari 1996]. "Sog'liqni saqlash kasblari to'g'risidagi qonun". Britaniyadagi Kolumbiyadagi haykallar va qoidalar. Vankuver, Britaniya Kolumbiyasi, Kanada: Queens Printer. Arxivlandi asl nusxasidan 2013 yil 25 avgustda. Olingan 2013-08-30.
- ^ "Bizning rolimiz". Hemşirelik va akusherlik kengashi veb-sayti. London, Angliya. 2011-08-31 [2010-02-24 da yaratilgan]. Arxivlandi asl nusxasidan 2013-09-05. Olingan 2013-08-30.
- ^ "Hamshiralar va akusherlarning buyrug'i 2001 yil". London, Angliya: Ulug'vorning ish yuritish idorasi, Milliy arxiv, Adliya vazirligi, Janob hazratlarining hukumati. 2002. Arxivlandi asl nusxasidan 2013-08-08.
- ^ Burton N (2015). Natal belgilar: homiladorlik, tug'ilish va ota-onaning madaniy namoyishlari. Demeter Press. ISBN 9781926452326. OCLC 949328683.
- ^ a b v d e Barbara R (2011). Rivojlanayotgan taqdirlar: Mayya doyasi va shahar. Oksford universiteti matbuoti. ISBN 978-0-19-531990-3. OCLC 779676136.[sahifa kerak ]
- ^ a b v Inge B (2006). Peru tog'li hududida bolalarni tarbiyalashni hurmat qilish madaniyatida o'sganman. Texas universiteti matbuoti. OCLC 748863692.[sahifa kerak ]
- ^ a b Dziadosz M, Basch RS, Young BK (mart 2016). "Inson amniotik suyuqligi: terapevtik foydalanish uchun ildiz hujayralarining manbai". Amerika akusherlik va ginekologiya jurnali. 214 (3): 321–27. doi:10.1016 / j.ajog.2015.12.061. PMID 26767797.
- ^ Vernon DM, tahrir. (2005). Avstraliyada buyuk tug'ilish: dunyoga yangi hayot olib kelgan ayollar va erkaklar yigirma tantana, kuch, sevgi va zavq. Kanberra, Avstraliya: Avstraliya doyalar kolleji. p. 56. ISBN 978-0-9751674-3-4.
Tashqi havolalar
![]() Rossiyada tug'ilgan 17 kilogrammli bola da Vikipediya
Rossiyada tug'ilgan 17 kilogrammli bola da Vikipediya
- O'z-o'zidan qin orqali etkazib berish, Merck Manual Professional Edition tomonidan tayyorlangan video
- [1] Onalik kasalligi / ommaviy axborot vositalarida o'lim
| Tasnifi |
|---|
